September 12, 2012
class warfare
The politics of austerity are alive and well in Victoria, NSW and Queensland. It is the essential services that cater for the more disadvantaged sectors of the community---health and education (including TAFE) --- at a time when income inequality has risen steadily in Australia since about 1980, and AustraliaŌĆÖs educational achievement is slipping.

Gonski argued that educational disadvantage is concentrated in the public school system and that the funding of the system exacerbates those inequities. The Gonski Review called for a big increase in funding to ensure that the growing equity gap between advantaged and disadvantaged communities is closed.
The other side of the politics of austerity is the attack on social justice--ie., the redistribution of resources to the poor and disadvantaged --as a form of class warfare and class envy in conservative political discourse. This politics here is to defend private health insurance and private education at independent schools.
So we have a winding back of the welfare state and to tell the poor to adapt to a transition to a health and education system that involves more personal responsibility and individual contributions. The rhetoric is that this wind back is necessary to avoid a debt burdened Queensland becoming like Greece.
Posted by Gary Sauer-Thompson at 8:39 AM | Comments (8) | TrackBack
August 30, 2012
dental reform, finally
The $4 billion dental care scheme targeted at low and middle income people is an excellent idea and long overdue. The government will provide Medicare funded dental services to children and an expanded public dental service for low-income adults and those in rural and regional areas, as well as an additional investment in dental infrastructure and workforce.
It is good public health policy as it is preventative and maintenance oral care in the community, even though it depends upon there being a private provider being willing to offer services in one's area at a price one can afford.

Outside health policy circles the reaction was more along the lines of the Gillard Government being on a spending spree, budget surpluses being blown out of the water, and the budget surplus for 2012-13 being a mirage.
The gigantic budget black hole scenario gives little acknowledgement of the Gillard Government making spending cuts in low priority areas to cover the budget surplus that is under pressure.
In the longer term there is the cost of the new higher priority programs ( the National Disability Insurance Scheme, which is expected to require an extra $10.5 billion a year within six years, the $4 billion dental care scheme, and the $5 billion a year for education recommended by the Gonski schools review) in the context of a mining boom that is winding down.
The argument is that ChinaŌĆÖs economic boom is showing signs of cooling, potentially torpedoing the federal governmentŌĆÖs revenue projections. Iron ore prices, a main ┬Łgenerator of government revenue, have tumbled below the level forecast by Treasury. The inference is that the days of the large surpluses being delivered by buoyant tax receipts are behind us and that the tax system will be unable to cope with new spending promises.
The political inference is the lack of fiscal discipline means new taxes to cover the budget deficit. That is, the Gillard Government is firmly in the tradition of big spending, high taxing Labor governments. They are bad economic managers--the familiar right wing riff.
Posted by Gary Sauer-Thompson at 10:18 AM | Comments (4) | TrackBack
August 16, 2012
Big Tobacco defeated
The Gillard government and public health advocates are deservedly celebrating the High Court recent decision on upholding plain packaging. This dismissed Big Tobacco's argument that plain packaging amount to expropriation of their trade marks and held that the plain packaging regime is valid under the Australian Constitution. The court has yet to release its reasons.
By December 1 this year, tobacco companies selling cigarettes in Australia will have to standardise the marketing of their cigarette packs in an ordinary olive-brown colour featuring large graphic health warnings with minimal space for their specific brand name. That may help to discourage smoking among young people--prevention of uptake of harmful products is a key strategy in public health.
 David Rowe
David Rowe
The Institute of Public Affairs (IPA) has been diligent in opposing regulatory restrictions on corporations--- paternalist government regulation that restricts individual liberty and responsibility. No doubt it will run its argument about the Nanny State --eg., plain packaging laws are an intrusive nanny state intervention designed to drive those Australians who still smoke off their drug of choice.
No doubt this think tank, which stands for free markets and limited government, will find new arguments to defend the interests of Big Tobacco, which has used the legal system to undermine public health policy that protects people from the deadly health effects of cigarette smoking.
The textbook tobacco industry objections to plain packaging are: it amounts to government seizure of trademarks; there is no evidence it will work; it will make counterfeiting easier. Big Tobacco will now seek to overturn the decisions of a democratic state by using international trading agreements and law (WTO).
Some trade agreements have clauses which allow foreign investors to sue governments, on the grounds that a law or policy ŌĆśharmsŌĆÖ their investment. There are provisions for member states to address public health concerns and to adopt measures necessary to protect public health.
Big Tobacco industry has been evasive in admitting liability for tobacco-related health harm and damage,
Posted by Gary Sauer-Thompson at 9:25 AM | Comments (7) | TrackBack
July 24, 2012
Australia: an obese nation
The ABC's Foreign Correspondent highlight the explosion of global obesity in places (China, India, Mexico, Brazil) where just a few decades ago hunger was a headline health concern.
Australia is also becoming an obese nation. Around 60% of Australians are overweight or obese, even though this epidemic only began around 1980? The consequence is increased risk of diabetes, heart attack and stroke, fatty liver, and breast and bowel cancer. Obesity has overtaken tobacco as the major burden of disease in Australia.

The reasons for this situation are two fold. The first lies in our food supply, which is highly processed, high fattening but very tasty and easy to get. The globalised food system generates a huge quantity of processed foods rich in fat, sugar and salt, which provide energy (calories or kilojoules) at very low cost. The energy-dense, nutrient-poor processed foods are much cheaper in terms of calories per dollar than are fresh minimally-processed foods that are the recognised basis of a healthy die--such as fresh plant foods, wholegrain cereals, lean meats and fish.
Secondly, there is inactivity through leisure-saving and entertainment technology such as cars, television, and computers. This points to action in areas that encourage incidental physical activity at the population level ŌĆō urban planning to encourage walking, cycling and the use of public transport and workplace innovations.
The financial pressures on the health system from the burgeoning burden of disease attributable to overweight and obesity will probably be the trigger to push governments into action. The processed food industry is an extraordinarily powerful and influential lobby in Australia and throughout the world. It successfully lobbied against traffic-light labelling in Australia and it will resist significant public health initiatives to address obesity.
Posted by Gary Sauer-Thompson at 11:59 PM | TrackBack
April 11, 2012
health reform: Medicare locals
A central strand in health reform under the Rudd/Gillard Labor Government is trying to shift the centre of gravity of the health system from hospitals to primary healthcare in order to achieve greater equity and to use resources more efficiently and effectively.
The vehicle being built to do this are the sixty-two new primary healthcare organisations known as Medicare Locals, which are being built from the current regional Divisions of General Practices across Australia to identify and plug the gaps in the current health care system.
They are a first step towards a more integrated health-care system. Their strength will lie in their ability to bring together a wide group of health service providers to address the communityŌĆÖs health problems.
Melissa Sweet in Medicare goes local in search of ŌĆ£disruptive innovationŌĆØ at Inside Story says that Medicare Locals are being asked to do what may well prove to be impossible: to be a type of super-bandaid patching together a fractured health system.
She says:
Their task is to integrate a fragmented primary care sector by helping GPs, practice nurses, psychologists, physiotherapists, community health workers, allied health professionals, pharmacists and others in the public and private sectors to work more closely with each other. In addition to roping together the silos within primary care, Medicare Locals are expected to develop better links between primary care and public and private hospitals as well as aged care services. They are intended as the glue in a system whose entrenched funding and structural divisions have not been budged by efforts at national health reform..Beyond all this, they are also charged with shifting the focus of primary care to population health.
I cannot see it happening myself. Medicare Locals don't have that much money and little authority to pull the patchwork of private primary care services into networks and to fill service gaps. GPs, for instance, are being asked to share power and influence and to see their own clinical practice and business models in a broader primary care context.
They wonŌĆÖt be in a position to address the chronic imbalance between hospital and community care, and given their birth in Divisions of General Practice, they won't have a broad vision of primary health care (ie., social and community health) that is necessary to help keep people out of hospital.
Posted by Gary Sauer-Thompson at 11:11 AM | Comments (4) | TrackBack
February 8, 2012
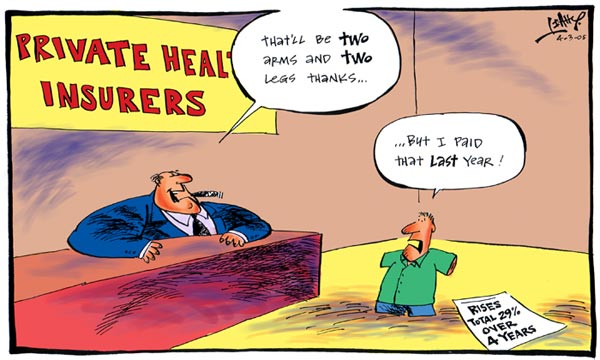
means testing private health insurance
The governmentŌĆÖs bill to means test private health insurance rebates for high-income earners is scheduled for debate on Thursday in the House of Representatives. Currently, anyone who takes out private health insurance receives a 30% government refund on their premiums, courtesy of the Howard Government. The Liberals finally came to accept Medicare but then used a succession of carrots and sticks to get people back into private health insurance.
 Diane Cordell
Diane Cordell
Under Labor's proposed scheme, singles with health insurance earning more than $80,000 and couples earning more than $160,000 would receive a rebate of 10% to 20%. Singles earning $124,000 and couples on $248,000 would no longer be eligible. The bill includes a penalty for higher income earners who donŌĆÖt take out private health insurance ŌĆō the Medicare levy surcharge.
These measure are part of Labor's agenda to roll back some of the middle-class welfare that Howard introduced to health and social security payments.
However, these measure have been knocked back by the Senate, mainly because of the Liberal Party who just love a big welfare state in spite of the small government rhetoric.
They also love the idea means testing welfare payments (welfare should be a safety net) but are opposed to means testing the private health insurance rebate. Hence they support the big social democratic welfare state they say they are deeply opposed to.
The proposals have the benefit of removing a glaring inequity in our present arrangements, which direct subsidies disproportionately to the well-off and underpin a middle class entitlement culture. Class war say the Liberals, even though the money saved could, and should, be used to improve public health services.
The policy issue here is that if we accept that private hospitals serve an important function, then they should be funded by means other than through private Insurance. Public funds for private hospitals should be paid directly to them, rather than being churned through private insurance where around 15 percent of that money goes in administration and profits. That would also be fairer to those Australians who pay for private hospital care from their own pockets, without being dependent on insurance.
Secondly, private health insurance is an expensive and clumsy way to do what the tax system and Medicare do so much betterŌĆēŌĆöŌĆēthat is to distribute funds to those who need health care.
Posted by Gary Sauer-Thompson at 3:50 PM | Comments (7) | TrackBack
January 17, 2012
Reforming Medicare
In his opinion piece----What is wrong with Medicare? ---in the Medical Journal of Australia Tony D Webber argues that the lack of audit control and inability to adapt to change leads to massive waste. He estimates that 2ŌĆō3 billion dollars are spent inappropriately each year.
One form the waste takes is the Medicare Benefits Schedule (MBS). This is riddled with misdirected incentives for practitioners, contains items that have not been reviewed despite advances in technology, and has many examples of good public policy thwarted by the MBS rules.
Webber, who is the Director of Professional Services Review that was established to protect the integrity of Medicare and the Pharmaceutical Benefits Scheme (PBS), says that:
In general practice, general practice management plans (GPMPs) and team care arrangements (TCAs) have created opportunities for a bonanza for some practices. Several practitioners I have reported on had admitted that their corporate owner had a business plan based on a defined number of these items claimed every week, irrespective of clinical need. Medicare Australia is also aware that a significant proportion of these plans are not carried out by a patientŌĆÖs usual doctorŌĆÖs practice.2 Anecdotally, claiming for clinically unnecessary GPMPs is significant throughout Australia. The policy intent of GPMPs was to provide a higher standard of care for patients with complicated chronic disease. While many doctors use these items appropriately for positive patient outcomes, a proportion of claimed items have added nothing materially to patient care.
Another form of waste that Webber highlights is the Howard government's Medicare Safety Net is one of the most poorly thought-through pieces of health legislation.
Despite its laudable policy intent ŌĆö to help those with severe and chronic disease afford the cost of modern medical care ŌĆö its implementation has gaping holes. The open-ended nature of the Safety Net offers the minority of unscrupulous and greedy practitioners opportunities to exploit it. After the Safety Net was introduced, a small group of obstetricians raised their fees for antenatal care from around $3000 to nearly $10 000. Such use of the Safety Net was perfectly legal, thanks to sloppily drafted legislation. During my time as Director of Professional Services Review, the Safety Net was used in effect to subsidise cosmetic procedures such as surgery for ŌĆ£designer vaginasŌĆØ at $5000ŌĆō$6000 each.The AMA, in responding to this criticism, accepted that there were some instances of abuse but argued that it was a matter of a few bad apples, common in every occupation, and not a systematic problem that runs through medical practice.
That response ignores a structural flaw in Medicare the GP as gatekeeper with respect to team care arrangements (TCA's). The policy intention was to allow patients with chronic or terminal disease to receive previously unaffordable care to allied health pratictioners (podiatry, physiotherapy, psychology, chiropractic). Unfortunately, the Department of Health and Ageing (DoHA)
developed MBS items that create incentives to easily misuse and work around the MBS requirements, leading to their misuse by a proportion of both medical and allied health practitioners. Some practitioners consciously misuse the MBS occasionally, and some do so regularly. The policy intent could have been achieved by allowing direct referral, without financial incentive to the doctor. This measure alone would have saved the health budget well over a billion dollars over the life of the program. Instead, a monster was created, eroding the integrity of the health budget.
The politics of medicine require that the GP act, and be paid, as the gatekeeper of Medicare.
Another structural flaw in Medicare arises from the changing health problems associated with a changing society. Jim Gillespie says that the Medicare system was designed for a younger society when the problems in the health system revolved around very short episodes of disease. You went to a general practitioner if you had a sniffle or some other minor complaint. And the fee-for-service system works very well with such occasional contacts. Hospitals worked on an entirely separate system that dealt with very serious illness.
Today we are living healthier, longer lives, but an ageing society brings with it a greater burden of chronic disease. Instead of short episodes of illness, ending in death or cure, this growing burden comes from serious and continuing illnesses, such as diabetes, chronic heart disease, and respiratory illnesses. These need continuity of care and management.
The structural flaw is that the Medicare universal insurance system wasnŌĆÖt designed to encourage continuity of care. Instead, it uses fee-for-service to fragment care into short episodes. Hence the need for reform. But the Australian health system is very hard to reform.
Posted by Gary Sauer-Thompson at 9:38 AM | TrackBack
November 10, 2011
News Ltd: ideology takes over
The Nanny State meme is a favourite of the News Ltd media, and it stands for an opposition to governmental policies of protectionism, economic interventionism, or strong regulation of economic, social, environmental and health. They have winner take all ethos, a political agenda, and they use their concentrated media power to push that agenda which includes destabilising the Gillard government.
One of the frequent targets of those on the right are the public health interventions to improve population health, especially those around cigarettes, gambling and adult and childhood obesity.

Gary Johns in Middle class should stop picking on poor, fat kids in The Australian states that the obesity crisis is a confected "crisis", as with gambling, smoking and drinking, where the middle class declares war on the underclass. He states that childhood obesity is apparently most prevalent in the lower classes (working class?) and more so among Aborigines, islanders and those from the Middle East.
Johns, to his credit, acknowledges that obesity is apparent and increasing, that it carries considerable health risks and costs, and that a core question is whether the cost of individual eating choices should be regarded as an individual or collective problem. He adds that the prevalence of obesity is not in dispute but its spread and policy responses are.
So what is his argument about those policy responses? It's not much:
For those on the Left of politics intervention comes easily. No doubt, they would be keen on a mandatory pre-commitment scheme where a child nominates the number of times each day they poke their head in the fridge. Or, maybe as part of income management, welfare recipients should receive fruit packages....The public health lobby presses for fat taxes and bans on junk food advertising. But these are ineffective and, besides, why should everyone have to suffer for the sake of the few? Preventive measures are justified only when there is strong evidence they pay for themselves... for society at large, labelling food or taxing selectively or banning advertising is a step too far.
Consumers don't need better information. Positive messages of good eating from teachers, doctors, nurses and an array of allied health workers, including nutritionists, will suffice.
Johns vaguely understands the social model of health, health inequity, and consumer control of health. He has a glimmer of understanding that this model means community control over the environmental influences of health, and that this is central to the shift required in the health system if real change is to occur. But he then resorts to mocking primary care and health prevention because ideology takes over: positive messages from government wont work but positive messages from health professionals will .
Posted by Gary Sauer-Thompson at 6:37 AM | Comments (12) | TrackBack
September 11, 2011
The Lancet on obesity
The Lancet has just run a series on obesity that explores its drivers, its economic and health burden, the physiology behind weight control and maintenance, and what science tells us about the kind of actions that are needed to change our obesogenic environment and reverse the current tsunami of risk factors for chronic diseases in future generations.
 Gary Sauer-Thompson, poster, MacDonalds, 2011
Gary Sauer-Thompson, poster, MacDonalds, 2011
The fact is, many Australians are fat and they are getting fatter.In the global obesity pandemic: shaped by global drivers and local environments paper, it is stated that:
The simultaneous increases in obesity in almost all countries seem to be driven mainly by changes in the global food system, which is producing more processed, affordable, and effectively marketed food than ever before. This passive overconsumption of energy leading to obesity is a predictable outcome of market economies predicated on consumption-based growth.The global food system drivers interact with local environmental factors to create a wide variation in obesity prevalence between populations... in high-income countries it affects both sexes and all ages, but is disproportionately greater in disadvantaged groups.
The primary cause is fast food and lack of exercise in an urban environment in which making healthy choices has become increasingly difficult.
The classical liberal view that individuals should make their own choices, free from state intrusion. According to this liberal account, the fact that your risk of being obese relates closely to your socio-economic status is not a question of social justice but a problem of the feckless poor being too ignorant or spineless to make good choices. Nudging us to healthier choices is OK, but regulating is not.
This view ignores the way that solutions to obesity and to improve health and development cannot be based on the existing framework (consumption-driven growth creating financially-defined prosperity) because this approach has helped to create the difficulties in the first place. Within this framework the fast food industry has become effective in its exploitation of basic human biological drives, desires, and weaknesses.
Posted by Gary Sauer-Thompson at 9:38 AM | Comments (2) | TrackBack
September 7, 2011
food labelling logic
A core strand of public health policy is directed at the 'development and implementation of cost-effective ways to reduce saturated, transfats, salt and sugar in foods by discouraging the production and marketing of unhealthy foods. The policy proposals aim to achieve smoke-free environments, restrictions on food marketing to children, increased alcohol tax and the promotion of generic medicines.
One proposal is food labelling in the form of front-of-pack ''traffic light'' labels on the food industry's products. This:
categorises the four key nutrients most associated with public health issues ŌĆō fat, saturated fat, sugars and salt ŌĆō as high, medium or low compared to the recommended level of intake of these nutrients.These ranks are portrayed as red, amber or green traffic lights on the package. Another light is sometimes included in the signpost for energy content, but it is not a core criterion.
The reason is that there is limited use of nutrition information currently presented on food packages. There is strong support for nutritional information to be placed on the front of food packages, particularly for nutrients that should be consumed in limited amounts, such as saturated fat, sugar, total fat and sodium. There are strong health arguments in favour of raising consumer awareness--informed consumer--- of what is in the food they buy.
The food industry in Australia (the Australian Food and Grocery Council [AFGC]) and elsewhere is strongly opposed to the traffic-light system. They prefer their Daily Intake Guide labelling (DIG), which is complex, difficult to understand and hinders consumers to make quick decisions about which is the healthiest product to buy.
The determination of the Australian food industry to avoid Traffic Lights is probably the surest indicator of their potential impact and we can expect that a big campaign to control public policy to suit their commercial interests. Food labelling is a huge issue for food multinationals ŌĆō it affects how their products are perceived by the customer, how well they sell. Mandatory labelling could put consumers off the products they sell.
We cannot have consumers overwhelmed with information can we? It would lead to consumer confusion and be a severe burden for manufacturers. So say the industry lobbyists. Any regulation should be industry-related not consumer-related.
Their aim is to occupy the food labelling ground first to show their commitment towards the public health and shape the debate from this position with their DIG scheme. We can expect the free market think tanks to provide the studies to support the food industry's position to reject plans for colour-coded traffic-light warnings. Parliament should obey the food industry's wishes and help block the consumer shift to locally produced and healthy food.
Posted by Gary Sauer-Thompson at 3:51 PM | Comments (1) | TrackBack
August 25, 2011
Gillard Govt: health reform
Credit where credit is due. The Gillard Government is currently besieged by the assaults around the Craig Thomson affair launched by the Coalition, which senses that an election is just around the corner. It is demanding an election right now. Apparently, the country is in crisis.
However, what is not being noticed is that the Gillard Government is a reforming government and that, in spite, of being on the electoral ropes, it is continuing with its programme of health reform.

The latest is the plain cigarette packaging legislation passed the House of Representatives in face of marked hostility from Australian tobacco industry that is controlled from London (British American Tobacco and Imperial Tobacco) and New York (Philip Morris) in order to to prevent similar measures from being introduced against its dangerous products in other countries.
The cigarette packs will now only show the death and disease that can come from smoking. Australia is actually taking a leadership role in global tobacco control, that is supported by the Coalition, in spite of the political donations it receives from Big Tobacco and the attacks launched by some of the ignorant crazies in the Coalition who claim that cigarettes are legal products and not harmful.
Other countries and other governments will now be encouraged by the Australian GovernmentŌĆÖs world-leading initiative to take on Big Tobacco's use of glamorous packaging as a way of advertising and promoting its products.
This highlights the importance of primary care ---a third of all cancers can actually be prevented through simple lifestyle choices like regular exercise, a healthy diet and quitting smoking.
Posted by Gary Sauer-Thompson at 2:50 PM | Comments (4) | TrackBack
July 23, 2011
orthodox + complementary healthcare
There is a debate over orthodox and complimentary health care at The Conversation. It doesn't get us very far from the tedious black and white (either/or) style of debate so common in Australia, even though pockets in the medical community seems to be growing more open to alternative medicineŌĆÖs possibilities, not less, despite the lack of clinical evidence supporting the claims of alternative medicine.
According to David Freedman in The Triumph of New-Age Medicine in The Atlantic the primary reason is because mainstream medicine itself is failing.The reason is that:
Modern medicine was formed around successes in fighting infectious disease.Infectious agents were the big sources of disease and mortality, up until the last century. We could find out what the agent was in a sick patient and attack the agent medically.ŌĆØ To a large degree, the medical infrastructure we have today was designed with infectious agents in mind. Physician training and practices, hospitals, the pharmaceutical industry, and health insurance all were built around the model of running tests on sick patients to determine which drug or surgical procedure would best deal with some discrete offending agent. The system works very well for that original purpose.
However, the success of modern medicine has bought to the fore the chronic, complex diseasesŌĆöheart disease, cancer, diabetes, AlzheimerŌĆÖs, and other illnesses without a clear causal agent. Now that we live longer, these typically late-developing diseases have become by far our biggest killers. Heart disease, prostate cancer, breast cancer, diabetes, obesity, and other chronic diseases now account for three-quarters of our health-care spending.
The drugs the medical profession thrown at these complex illnesses are by and large inadequate or worse, as has been thoroughly documented in the medical literature. The heavily prescribed drugs that have failed to do much to combat complex diseases, while presenting a real risk of horrific side effects. Many healthy people each year are converted into long-term patients.
The medical profession knows perfectly well what sort of patient-care model would work better against complex diseases than the infectious-disease-inspired approach weŌĆÖve inherited. That is one that doesnŌĆÖt wait for diseases to take firm hold and then vainly try to manage them with drugs, but rather is a preventive approach that focuses on lowering the risk that these diseases will take hold in the first place. This preventative primary careincludes the promotion of a healthy diet, encouragement of more exercise, and measures to reduce stress which impairs the immune system, rather than drugs and surgical procedures.
Freedman says that the latter involves a healing approach that is rooted in closer practitioner-patient interactions--a more caring practitioner who takes more time and bonds better with patients---focused on getting a patient to adopt healthier attitudes and behaviors interactions. This is not possible with the corporate approach to medicine in which GP's are paid for providing treatments, not for spending time talking to patients. Hence the shift to integrative health care--the conjunction of complementary with mainstream medicine.
This undercuts the either orthodox or complementary medicine approach since the middle ground is one of plugging the gaping holes in modern medicine and doing what is best for the patient. Alternative or complementary medicine is a legitimate response to mainstream medicineŌĆÖs real shortcomings.
Posted by Gary Sauer-Thompson at 8:25 PM | Comments (4) | TrackBack
July 21, 2011
health inequalities
In Australia overweight and obesity have become increasingly more prevalent among socially disadvantaged groups, particularly in urban areas. Like most other risk factors for ill-health, excess body weight tends to be more prevalent among people further down the social and economic scale.

Gary Sauer-Thompson, Mill St, Adelaide, 2011
Encouraging healthy eating habits is difficult given the extensive array of convenience and pre-packaged foods high in fat, sugar and salt (so called junk foods) which are increasingly available across the world, often promoted in large or multiple serving sizes.
This has made eating healthily a challengeŌĆöfor individuals personally, and for policymakers indirectly; and the challenge has been compounded by a bombardment of marketing and advertising that surreptitiously and adversely influences peopleŌĆÖs food preferences and consumption patterns.
In Overfed, overgrazed and difficult to overcome in the Sydney Morning Herald Elizabeth Farrelly refers to Sydney's diabetes map. This:
map reveals a clear doughnut pattern with dark, congealed patches around the west and exurban fringes (Mt Druitt, Wollongong, Toongabbie) and pale bits in the old centre (north shore, city, Coogee). It's the direct inverse of how a rickets or tuberculosis map would have looked a century ago.It's not just fat. Maps of obesity, heart disease, renal failure, smoking, TV-watching and hypertension - diabesity, if you'll excuse the coinage - would show similar patterns...What's interesting is that this stuff is class-related. Diabesity is a poverty indicator.
The data provokes the question not only why the poorest of the poor and the most vulnerable and marginalised groups have bad health but why is there a socially graded relation between social position and health?
The Marmot Review highlights that there is a social gradient in health ŌĆō the lower a personŌĆÖs social position, the worse his or her health. Health inequalities result from social inequalities. Consequently, reducing health inequalities is a matter of fairness and social justice. Health equity then becomes a marker of successful development.
So why the social gradient in health? Farrelly says that (relatively) poor Australians, despite decades of education campaigns, still see conspicuous consumption - of land, leisure, energy, alcohol, food - as a norm, not a mortal danger. It's overconsumption that is driving obesity and diabetes.
The problem with Farrelly's argument is that obesity and diabetes doesn't come from overconsumption per se (the middle class also over consume as Farrelly acknowledges); it comes from overconsumption of cheap junk food. What, and how much, people eat, drink and smoke and how they expend energy are responses to their socio-political, socio-economic, socio-environmental and socio- cultural environments.
From another perspective that a significant proportion of the Australia population now eats large volumes of energy-dense nutrient-poor foods--junk food --- does not expend enough energy, smokes and consumes harmful quantities of alcohol is a sign of success ŌĆōthe commercial success of the corporate food industry. It's a lucrative business. Hence the intensive advertising.
Posted by Gary Sauer-Thompson at 9:32 AM | Comments (13) | TrackBack
June 20, 2011
Medicare locals + health care
The Federal Government has announced the final boundaries for an Australia-wide network of 62 Medicare Locals. The reform vision behind this was for:
less micromanagement by Canberra and the States, greater flexibility through block funding arrangements, local community led primary health care organisations that understood the needs of their constituency, determined the best method of delivering services and went about their business. The notion of CanberraŌĆÖs ŌĆśone size fits allŌĆÖ approach where the funding arrangements gave much the same money and proposed the same model of care to deliver a mental health service to a middle class white patient in Penrith as it did to an Ngaanyatjarra Aboriginal patient from the Central Desert was meant to be dead in the water. Regional differences such as morbidity and mortality rates, access to resources, the cost of those resources, cultural differences, the need for outreach services, housing, education, employment ŌĆō the social determinants of health - were to be the new approach.
As expected, this vision of primary health care resulted in professional tussles over the roles and influence of GPs, nurses and pharmacists and who would run the Medicare locals. The Australian Medical Association has been agitating loudly for a ŌĆ£leadership roleŌĆØ for GPs in opposition to those interested in developing a more community-centred approach.
Realistically the community approach was never going to get off the ground, but what was hoped was that there would be a greater inclusion of allied health professionals, a shift away from the medical model of disease to a wellness model; and a greater emphasis on illnesses such as diabetes, hypertension, obesity, mental health and trauma, violence and substance abuse.
It is unlikely that the Medicare Locals will generate anything like this approach to health care, and it may be that it only come if communities and health practitioners develop it themselves, independent of the formal structures in the health system. The formal structures are shaping the content of Medicare locals.
Firstly, it is increasingly apparent that the Federal Government has capitulated on the issue of level of primary health care funding and is leaving the States to run primary health care services through their existing community and population health organisations with no promise of reform in health care.
Secondly, the Medicare Locals have lost their independence to the top down approach. As Lohengrin highlights the:
forerunner Medicare Locals which were formerly autonomous of Government, as most were independent locally managed organisations, will be nationalized, becoming regional offices of the Department of Health and Ageing. Their former independence of Government, able to lobby vigorously of behalf of their constituency, influence health policy and help drive continuing health reform will be neutered and potentially replaced by a new set of overly regulated, unresponsive, frustrated minions of the Government in Canberra, albeit with an office in your town.
So it is going to be more of the same kind of health care even though community health requires so much more than providing medical services. It is community health that the social determinants of health and health inequality come to the fore.
Posted by Gary Sauer-Thompson at 10:54 AM | TrackBack
June 4, 2011
mental illness
In The Epidemic of Mental Illness: Why? in the New York Review of Books Marcia Angell refers to the raging epidemic of mental illness in the US. We could say the same for mental illness in Australia in that about 20% of adult Australians, will experience a mental illness at some stage in their lives: and that many will live with more than one mental illness at a time, such as anxiety and depression, which commonly occur together.
Angell highlights:
the shift from ŌĆ£talk therapyŌĆØ to drugs as the dominant mode of treatment coincides with the emergence over the past four decades of the theory that mental illness is caused primarily by chemical imbalances in the brain that can be corrected by specific drugs. That theory became broadly accepted, by the media and the public as well as by the medical profession, after Prozac came to market in 1987 and was intensively promoted as a corrective for a deficiency of serotonin in the brain.
This diagnosis--that mental illness is caused by a chemical imbalance in the brain---has resulted in the pharmaceutical companies selling psychoactive drug through various forms of marketing, both legal and illegal, and what many people would describe as briberyŌĆöhave come to determine what constitutes a mental illness and how the disorders should be diagnosed and treated.
He asks:
What is going on here? Is the prevalence of mental illness really that high and still climbing? Particularly if these disorders are biologically determined and not a result of environmental influences, is it plausible to suppose that such an increase is real? Or are we learning to recognize and diagnose mental disorders that were always there? On the other hand, are we simply expanding the criteria for mental illness so that nearly everyone has one? And what about the drugs that are now the mainstay of treatment? Do they work? If they do, shouldnŌĆÖt we expect the prevalence of mental illness to be declining, not rising?
In his two part review of 3 recent books on mental illness Angell endeavours to answer these questions.
The first part of the article argues that psychoactive drugs are useless, or worse than useless because of their negative side effects. He then asks why are these drugs so widely prescribed by psychiatrists and regarded by the public and the profession as something akin to wonder drugs?
Posted by Gary Sauer-Thompson at 8:27 PM | Comments (2) | TrackBack
May 28, 2011
playing the cards badly
I watched Question Time in the House of Representatives last week and discerned a bit of shift in the flow of the conflict. The Gillard Government was less on the defensive fending off the assaults from the Coalition and more on attack.
The shift was partly due to the Coalition's attacks lacking punch. However, the shift was largely due to Nicola Roxon, the Health Minister, successfully taunting and tarnishing the Coalition as supporting Big Tobacco (British American Tobacco or Phillip Morris). The perception she was able to create is that the Coalition is in the pocket of Big Tobacco. Perception is everything in politics.

Roxon was able to harm the Coalition. The plain cigarette packaging legislation will pass the House of Representatives with the support of the crossbenchers and will it go to the Senate after July 1 when the Greens will have the balance of power. So the bill, which has widespread public support, will be enacted this year.
Yet the Coalition continues to oppose plain packaging -- which means that its opposition for oppositions sake results in the Coalition opposing good public health policy aimed at harm minimization, stopping people from starting to smoke, and reducing the health costs due to the harm caused by smoking. The nanny-statism around this rhetoric around the National Preventive Health Strategy looks empty on this issue--this is a toxic product; it is lethal.
This issue highlights the problem with Abbott's saying no to everything and slogans--stop the boats, cut the taxes, pay back the debt---strategy. The sky won't a fall in when the carbon tax is passed and Abbott will begin to look more naked.
Posted by Gary Sauer-Thompson at 10:57 AM | TrackBack
May 18, 2011
Liberals side with Big Tobacco?
The Liberal's election strategy of saying no, stoking the fear in the electorate, and blaming the carbon tax for everything to do with the cost of living has been effective. It is Abbot's agenda that is centre stage. Labor has lost confidence and looks punch drunk. The consensus amongst the Canberra Press Gallery is that Gillard Labor is finished. We are watching the death throes.
But there are limits to this kind of relentless negativity. This can be seen around the issue of preventative health care, most notably the policy attempts to reduce smoking. The latest government policy is cigarettes in plain packages (plain cigarette packs will become a mandatory olive brown on July 1, 2011). This is designed to reduce the effectiveness of the branding (wealth, cool, sophisticated) of cigarettes by Big Tobacco.
The rationale is to reduce smoking amongst the population as this continues to be Australia's largest preventable cause of death and disease.(eg., excess risk of premature birth, cardiovascular disease, respiratory disease and cancers of the respiratory, digestive and reproductive organs).

Big Tobacco is outraged. They are threatening legal action and to flood the market with cheap cigarettes. The appear to be fighting to defend a type of intellectual property called package branding.
Tony Abbot's strategy of saying no to everything has led him to support Big Tobacco and to oppose preventative health care. The line that Abbott is running is close to Big Tobacco's song sheet --that there was no proof plain packaging would reduce smoking rates, and that it would be counter productive because counterfeiters and organized crime will have a field day mass-producing packets to smuggle into Australia.
Abbott has sided with an industry that has historically shown no interest in people's health or wellbeing. It's product is toxic and Big Tobacco which has a long history of legislative challenges eg., the health warnings on packages. He is tacitly supporting the immorality of marketing a deadly product.
The history of tobacco control in Australia shows that smoking in the population as a whole will not reduce without vigorous and consistent action by governments and health organisations through Increases in the costliness of cigarettes, and large increases in media campaigns and the strong push towards smoke-free environments. They do so to because the diseases caused by smoking help drive exponential growth in spending on hospital, medical and pharmaceutical treatments in Australia.
Tobacco control in Australia has seen a 30% decline of smoking between 1975 and 1995. This has prevented over 400,000 premature deaths and saved costs of over $8.4 billion. 17% of Australians smoke. The evidence that half of them will die from doing so is no longer contested, even by the tobacco companies.
That comes to about 15,000 Australians every year who die from smoking-related diseases.
Yet Abbott sides with Big Tobacco! That is where the relentless attack Gillard and her government on everything they do has lead him. So where is the political advantage in being seen to side with Big Tobacco?
Posted by Gary Sauer-Thompson at 9:20 AM | Comments (18) | TrackBack
May 8, 2011
being blue
An example of how our era when biologicalŌĆöand specifically, geneticŌĆöcausation is taken as the preferred explanation for all human physical differences.
The announcement in February 2001 that two groups of investigators had sequenced the entire human genome was taken as the beginning of a new era in medicine, an era in which all diseases would be treated and cured by the replacement of faulty DNA.
For nearly ten years announcements of yet more genetic differences between diseased and healthy individuals were a regular occurrence in the pages of The New York Times and in leading general scientific publications like Science and Nature. There have been an increasing number of medical books analysing the concepts of health and disease from the perspective of evolutionary biology
In ItŌĆÖs Even Less in Your Genes in the New Review of Books Richard C. Lewontin observes that:
the search for genes underlying common causes of mortality had so far yielded virtually nothing useful. The failure to find such genes continues and it seems likely that the search for the genes causing most common diseases will go the way of the search for the genes for IQ.
The idea that emotional distress is due to an underlying organic disease downplays the effects of negative life circumstances or acute trauma and non-biomedical accounts of mental distress and disorder.
He adds that:
Experimental geneticists, however, find environmental effects a serious distraction from the study of genetic and molecular mechanisms that are at the center of their interest, so they do their best to work with cases in which environmental effects are at a minimum or in which those effects can be manipulated at will. If the machine model of organisms that underlies our entire approach to the study of biology is to work for us, we must restrict our objects of study to those in which we can observe and manipulate all the gears and levers.
The biomedical model of medicine holds that health constitutes the freedom from disease, pain, or defect, thus making the normal human condition "healthy". The model's focus on the physical processes, such as the pathology, the biochemistry and the physiology of a disease, and does not take into account the role of social factors or individual subjectivity.
This failure stems partly from three assumptions of the biomedical models: all illness has a single underlying cause; disease (pathology) is always the single cause; and removal or attenuation of the disease will result in a return to health. The assumption that a specific disease underlies all illness has led to medicalisation of commonly experienced illnesses as opposed to disease resulting from cellular abnormalities.
Posted by Gary Sauer-Thompson at 10:31 PM | Comments (1) | TrackBack
February 16, 2011
health reform: more local control
The National Health Service (NHS) in the UK is becoming dysfunctional and causing harm to elderly patients. And so we have the market-based reforms from the Cameron Government:
 Martin Rowson
Martin Rowson
A radical argument for health reform is made by Simon Jenkins in The Guardian. His diagnosis of what has gone wrong with the NHS is that it is too big. His solution is that somehow local responsibility must be rekindled and that GPs and their surgeries must regain the initiative.
He says:
Aneurin Bevan was wrong to nationalise it back in 1948. Morrison was right in wanting a new health service based on charitable and municipal hospitals, as almost everywhere else in the world....Bevan wanted "a maximum of decentralisation to local bodies and a minimum of itemised central approval". He got the opposite....It is significant that every attempt to reform the NHS tries to break it up, by denationalising, regionalising, introducing market forces, contracts, choice, anything to reduce bulk. Each attempt fails. The only conclusion no one dares mention is that the rest of the world was right and a "national" health service is too big....Schumacher was right. Big is ugly. NHS gigantism is like the Pentagon. Its interests are too institutionalised, its lobbyists, especially the doctors, too powerful, and its internal controls so pervasive as to seize up the system.
He adds that all arguments about the state of the NHS on the left, are predicated on the maxim that it must have more central accountability and control. The way to improve hospital care is to castigate the minister, shriek postcode lottery and demand money with menaces. Big is best.
The turn to localism is made in Australia by Armstrong, Woodruff, Legge and Wilson in their Putting Health in Local Hands in whoch they propose the establishment of local Regional Health Organisations (RHOs) across Australia, with each responsible for the health care needs of a defined population within their region:
This model proposes that all current health care funding from local, state and federal governments be pooled within a national agency and equitably distributed to RHOs on the basis of evidence about health care needs. Publicly available information on local health needs and health spending (regularly collected and updated in accordance with national standards) would inform decisions by RHOs about the appropriate allocation of services and resources in that region.
This is the opposition of the centralization model favoured by Rudd and which was premised on the Commonwealth having a controlling share in hospital funding and a Commonwealth primary care takeover. Thus the Commonwealth has majority funding responsibility for the entire health sector.
Posted by Gary Sauer-Thompson at 5:07 PM | Comments (3) | TrackBack
February 15, 2011
Gillard's art of compromise
In the Sydney Morning Herald Geoff Gallop argues that Gillard is a facilitator who works to build consensus for change. With reference to health reform he says:
Gillard had a decision to make ŌĆō should she plough ahead with the initial plan [that proposed that states and territories give up a portion of the GST] or should she start again? By starting again she was able to get Western Australia and the new government in Victoria into the tent. She listened and they responded.. Leadership is not just strength in the face of conflict but also agility in the face of difference. This requires emotional intelligence as well as political awareness. In other words it is about judgement as well as strength. It is about knowing when to push forward, when to hold your ground and when to take a backward step.
Gillard did this. Gallop says that the Heads of Agreement on National Health Reform signed between the federal government and the states and territories on Sunday represents a significant achievement for Prime Minister Julia Gillard. She managed the traditional Commonwealth versus States/Territory COAG conflict and it was a win for the Prime Minister.
Is it a significant achievement in terms of health reform?
Gallop is right about Gillard's negotiating skills: she is skilled in the art of negotiation and compromise. However, these skills are only useful if they can be deployed to achieve reform to make things better. Therein lies the problem: it is a very small step on the slow road to change.
What was delivered was not health reform. Gillard backed down on the federal government be the dominant funder; backed down on federal funding of 100 per cent of primary care; did not explicitly address the insufficient focus on prevention and primary care in the health system; and did not address the fragmentation that exists at present between hospitals and primary care services.
The emphasis in the new reform plan is about hospital funding.The Commonwealth has accepted the states should retain control over hospitals and that the Commonwealth will have ''no role, directly or indirectly'' in the negotiations by state governments to establish local hospital network services. The states continue to run the hospitals with the federal government guaranteeing to pay 45 per cent of the increase in public hospital costs from 2014, then 50 per cent from 2017.
The states and the commonwealth basically argue that the big problem is the health system is running out of money when the real problem, as Tim Woodruff points out, is that there is no system:
Patients are faced with the nightmare of negotiating the public hospital system, the publicly subsidised private hospital system, the general practitioner system, the community care system, the publicly funded private allied health system, the mental health system, the publicly subsidised private dental system, the public dental system, the aged care system, the private specialist system, the public specialist outpatient system, and a myriad of other poorly connected pieces.
Structural reform to integrate these systems is required, but is not suggested in this plan. What we have is relatively powerless regional organisations---Medicare Locals--- being charged with co-ordinating this maze of primary care services. the Commonwealth's backdown on taking over all primary care funding means that an added barrier to co-ordination will be a continuation of different sources of funding.
Update
The reform of hospital services that are designed to make them more efficient and so better for patients are:
(1) local hospital networks made up of small groups of local hospitals that collaborate to deliver patient care, manage their own budget and are held directly accountable for their performance. This will avoid the fragmentation and duplication that would come from individual hospitals operating independently from other hospitals in their area,
(2) a four-hour waiting time target for emergency department patients. This involves providing $500 million in funding from 1 July 2010 to ensure patients are admitted, referred or discharged within four hours of arriving at an emergency department, where clinically appropriate.
(3) an elective surgery access guarantee designed to reduce the numbers of patients kept dangling on lists, in some cases for well over a year coupled to providing $650 million to fast-track elective surgery patients who have been waiting longer than clinically recommended;
(4) activity-based funding, or casemix, which will work by assigning a notional "efficient price" to each operation and service hospitals provide.
I'm not sure that these will necessarily lead to better patient care in hospitals--though they are steps in the right direction. Activity -based funding, for instance, does mean the government is starting to pay hospitals for what they do deliver.
The old model of block government funding meant that an increase in patient numbers was bad news for hospitals because they had to eke out their budgets further to treat them all.Their response was get patients out of hospital quickly and shifting the costs on to the non-hospital sector.
Posted by Gary Sauer-Thompson at 11:25 AM | Comments (8) | TrackBack
February 4, 2011
fatism
Food and everything that surrounds it is a crucial matter of personal and public health. Changing sedentary, high-cholesterol, high blood pressure, high blood sugar fat people into more active, low-cholesteral, normal blood pressure, normal blood sugar fat people improve their health and wellbeing.
We can see from this on John Birmingham's Why is fat such a fractious issue? in the Brisbane Times in which it is mentioned that obesity skews significantly towards the lower income groups for a whole bunch of reasons.
In an earlier post --A weighty issue----Birmingham writes that from his own painful experience personal responsibility for what you eat and how you burn off any excess energy is, for a lot of the population, one hundred percent of the issue. He then asks:
Is it inevitable as the rate of obesity increases in Western society, that obesity will come to be defined as the norm? I ask that as somebody who has been obese. Not just clinically obese. But morbidly obese. I'm not any more, but only because I got so sick at one stage from carrying that much weight, that I suddenly dropped a couple of kilos and decided to kick on and see if I could get rid of the rest of it. I was very lucky in having both the money and the time to be able to do so. Not everybody does.
He wonders whether or not obesity might well become as politically fraught in the near future as smoking has become over the past decade. Will it get to a point where the word 'fat' is no longer considered appropriate in polite circles, because of the offence and hurt it might cause?
Even though obesity is deadly and crippling and is killing people Birmingham's answer is that there a concerted effort to 'normalise' fat as a condition in the form of the 'human right' to be fat, not to feel bad about it and to contest the argument that obese equates to being unhealthy.
Obesity is a public health issue, so a policy response is appropriate, but there won't be much of one, because of the power of the food industry. The situation is that we sell junk food while telling people not to eat it.
Despite our our diet being unhealthful and unsafe it is highly unlikely that there will be a tax on junk or high processed food food; or that government subsidies to processed food are ended; that Agricultural Departments whose goal is to expanding markets for agricultural products for junk food become an agency devoted to encouraging healthy eating; factory animal feeding operations are discouraged whilst encouragement is given to the development of sustainable animal husbandry; provide food education for children in public schools as part of the national curriculum; mandate truth in labeling.
Even though public health is an accepted role of government, the reaction to the above would be that this is nanny-state paternalism ; that itŌĆÖs time we ŌĆ£stop harassing people about their weightŌĆØ; and that we are in the midst of a moral panic.
Posted by Gary Sauer-Thompson at 1:07 PM | Comments (8) | TrackBack
January 18, 2011
austerity politics
As I've mentioned in previous posts the politics of austerity is in full swing in Europe where it is targeting the welfare state. In Britain it is the National Health Service that is being targeted:--- the reforms of the Conservatives and Liberal Democrat Coalition mean that the new private entrants grow at the expense of the old state ones.
 Martin Rowson
Martin Rowson
It is Schumpter's process of creative destruction organized by a neo-liberal state. As the NHS budget shrinks, as new providers enter the market, some old ones will have to go to the wall. The new act gives the health secretary no authority to intervene: price competition, enforced by EU law, will alone ordain which services live or die. The market will be used to ensure that weak providers are forced out.
The hard edge to this politics of austerity is highlighted by Paul Krugman in reference to the politics espoused by the Republican Party in the US with respect to the reform the private health insurance system:
The key to understanding the G.O.P. analysis of health reform is that the partyŌĆÖs leaders are not, in fact, opposed to reform because they believe it will increase the deficit. Nor are they opposed because they seriously believe that it will be ŌĆ£job-killingŌĆØ (which it wonŌĆÖt be). TheyŌĆÖre against reform because it would cover the uninsured ŌĆö and thatŌĆÖs something they just donŌĆÖt want to do. And itŌĆÖs not about the money. As I tried to explain in my last column, the modern G.O.P. has been taken over by an ideology in which the suffering of the unfortunate isnŌĆÖt a proper concern of government, and alleviating that suffering at taxpayer expense is immoral, never mind how little it costs
This harshness is what I find hard to accept, especially when most people who are underinsured or uninsured today in the US are hard working, tax paying, currently employed people. Some have lost coverage due to the loss of a job during the economic crisis, but they are actively seeking employment, they aren't just lazy and wanting a free ride. They are self-employed, work for a company that doesn't offer health benefits, or live pay check to pay check and simply can not afford the rapidly rising cost of insurance or healthcare in the US.
Fifty million uninsured, the highest per-capita costs in the world, millions of people pushed into bankruptcy by medical bills, worse health outcomes than most of the industrialized world? Fundamental healthcare should be part of the social safety net in which in which affordable and universal healthcare is a given.
This is opposed because one of the Republican Party's tacit political principles is inequality. They accept that health care should be controlled by an team of insurance-company bureaucrats, whose bonuses and promotions depend on denying your claims and limiting your care.
Posted by Gary Sauer-Thompson at 11:23 AM | Comments (2) | TrackBack
December 2, 2010
Health reform: states reneg?
National health reform has become more complex with the new Baillieu Government in Victoria threatening to back out of the COaG deal the Rudd/Gillard Government had signed with the states. This involved the states handing back one-third of their stateŌĆÖs GST revenue in return for increased funding and a guarantee that the Commonwealth will fund 60 per cent of hospital costs. Apparently the NSW Liberals threaten to follow the Baillieu Government.
I'm unsure of the reason for this, given the spiralling costs of running the public hospital system, or what the proposed alternative would be. I would have thought that the core strategy for the Liberal states (WA, Victoria, NSW) is to obtain real growth in federal funding for the public hospital systems over the next decade. This position assumes that the Liberal states want to maintain the Medicare policy of universal access to comprehensive public hospital services (that is their stated policy position).
Jeremy Sammut, a research fellow at the Centre for Independent Studies, thinks otherwise in his Ridicule the prescription to induce health reform at the ABC's Unleashed. He radically questions the policy consensus on the long-term sustainability and bipartisan political desirability of Medicare.
He says that we need to:
go back to first principles and admit the original error which, of course, was the decision to establish a government-run health system in the first place....Hospital care needs to be treated like any other good the community desires. It needs to be purchased by or on behalf of patients from providers who compete to deliver these services at the efficient cost of production.The health fund an individual joins to insure themselves against the risk of serious illness should be responsible for doing the purchasing. Each fund should be free to purchase services from the public or privately-owned facility that is able to deliver the best quality care at the best price. Artificial restrictions on hospital bed numbers would not exist in such a system in which the supply of hospital care was demand-driven.
What is necessary is real structural health reform--the key is not health delivery but health insurance not health delivery. To achieve it, Sammut says, the myth of ŌĆśfreeŌĆÖ hospital care needs to be busted. We know there is not enough money in the economy for governments to pay for all the hospital care required each year. Hence the need to restrict or ration access to hospital care.
We therefore need to fund hospital treatment overtime by paying for insurance premiums. Medicare should be scrapped and the ŌĆśrightŌĆÖ to taxpayer-funded health care replaced with a health voucher. Each Australian would use their taxpayer-funded voucher to purchase private health insurance.
Genuine health reform is dumping social democracy's Medicare, that is premised on health care as a core government service and responsibility, and embracing the neo-liberal's free market profit driven approach to privatised health care.
An alternative approach going back to first principles is to rethink the way that health care is reduced to hospital or emergency care. The costs of hospital care can be reduced by keeping people out of hospital by investing in preventative primary care, so that people do not need to end up in emergency departments of hospitals. That too is structural reform.
In arguing for his market-based approach Sammut neglects to mention that it is the market failure in health care that requires government intervention in the form of Medicare. Nor does Sammut mention the large public subsidy of the private health funds through the mechanism of the private health insurance rebate. This was introduced by the Howard Government to ensure a consumer shift to private health insurance to help the health insurance industry stay afloat.
The problem the Gillard Government faces is that Labor under the previous Rudd/Gillard government got sidetracked in its reform of the health system by placing the emphasis on the funding of hospitals; and away from strengthening the relationship between preventive care and hospital care. Sidetracked because from federal Labor's perspective it is the relative isolation of the general practitioners that they fund from the rest of the system needs to be addressed. Federal Labor had proposed to do this with a national network of primary health care organisations to be known as Medicare Locals.
Consequently, the current debate on national health reform has been reduced to one about hospital funding, not better health care through developing a more functional nexus between hospital and community health and primary care services.
Posted by Gary Sauer-Thompson at 10:39 AM | Comments (10) | TrackBack
July 15, 2010
Big Pharma + academic medicine
Marcia Angellm, the former editor-in-chief of the New England Journal of Medicine, has an article in the Boston Review on BIg Pharma and academic medicine. It is part of a series of articles or a forum run by the Boston Review on the impact of the pharmaceutical industry on medical training and science, and the responsibilities of physicians.
Angellm's argument is that financial conflicts of interest are a serious impediment to good medical research, education, and clinical practice. She says:
Over the past two or three decades....academia and industry have become deeply intertwined. Moreover, these links, though quite recent, are now largely accepted as inherent in medical research. So whatŌĆÖs wrong with that? IsnŌĆÖt this just the sort of collaboration that leads to the development of important new medical treatments?
She answers thus:
Increasingly, industry is setting the research agenda in academic centers, and that agenda has more to do with industryŌĆÖs mission than with the mission of the academy. Researchers and their institutions are focusing too much on targeted, applied research, mainly drug development, and not enough on non-targeted, basic research into the causes, mechanisms, and prevention of disease.
In addition to distorting the research agenda, there is overwhelming evidence that drug-company influence biases the research itself, primarily suppression of negative results.
She adds that one consequence is that doctors and their patients come to believe that for every ailment and discontent there is a drug, even when changes in lifestyle would be more effective. Big Pharma hires physicians to sell diseases.
No doubt ageing will be sold as a disease/illness state and we will be bombarded by anti-ageing messages with supplements and hormone treatments by anti-ageing medicine that is fast becoming big business. Anti-ageing medicine is dismissed as quackery by orthodox medicine--eg., on the use of growth hormone therapies in anti-aging medicine--- but orthodox medicine does turn a blind eye to its own corruption by Big Pharma, or the way that orthodox medicine is a business.
Posted by Gary Sauer-Thompson at 11:07 AM | TrackBack
June 18, 2010
huh?
What is wrong with the Rudd Government? On the one hand, we have the passage of paid parental leave legislation that provides a mandatory paid leave for new parents (18 weeks of leave paid at the national minimum wage) for the first time. On the other hand, we have the removal of the National Funding Authority for health.

Remember how the $50 billion health and hospitals package was sold as an example of co-operative federalism, the biggest reform since Medicare, and an example of how Rudd Labor could solve the nation's health crisis? This reform package is now being undercut with the dismantling of the National Funding Authority, which was to oversee the distribution of Commonwealth health funding to the states.
Plans for the National Funding Authority were agreed to by Prime Minister Kevin Rudd, and also by premiers at the Council of Australian Governments summit on health reforms in April.The authority had been proposed to ensure health funding transparency between the Commonwealth and the states.If it has been dropped because it is not needed, then the health funding arrangements were not thought through.
Do I detect the hand of the NSW Right (Karl Bitar and Mark Arbib) here? One strong on (focus group) politics and weak on policy? Where is the strategy in health reform? What has happened to the challenge to the special interests of state governments and their health bureaucracies? There is little chance of establish a permanent, independent, professional and community-based statutory authority, an Australian health commission, similar to the Reserve Bank in the monetary field.
We know that after the collapse of the Copenhagen climate change talks and the decision of the Coalition to withdraw its support for the government's ETS, the Greens proposed adopting an interim arrangement - proposed by the government's own climate change advisor Ross Garnaut - which would have imposed a relatively small carbon tax until a more substantial price mechanism for carbon emissions could be agreed.The government however refused to discuss the proposal with the Greens.
What next in the roll back of reform?
We have the "education revolution" but it isn't going that far to address the negative effects of the inequality caused by globalization. Over the last 20 years that inequality has a consistent geographical spread in Adelaide and it is inter-generational.
Posted by Gary Sauer-Thompson at 12:25 PM | Comments (13) | TrackBack
May 29, 2010
food politics
In The Food Movement, Rising in the New York Review of Books Michael Pollen, an ethical food guru, says that, if the advent of fast food (and the culture of cheap processed food in general) has become an indispensable pillar of the modern economy, then it has given rise to criticism that industrial food production (agri-business) is in need of reform because its social/environmental/public health/animal welfare/gastronomic costs are too high.
Public health is central given the current concern about the health of the population:
perhaps the food movementŌĆÖs strongest claim on public attention today is the fact that the American diet of highly processed food laced with added fats and sugars is responsible for the epidemic of chronic diseases that threatens to bankrupt the health care system. The Centers for Disease Control estimates that fully three quarters of US health care spending goes to treat chronic diseases, most of which are preventable and linked to diet: heart disease, stroke, type 2 diabetes, and at least a third of all cancers. The health care crisis probably cannot be addressed without addressing the catastrophe of the American diet, and that diet is the direct (even if unintended) result of the way that our agriculture and food industries have been organized.
The food industry's claims, that it merely giving people the sugary, fatty, and salty foods consumers want, ignores that it actually helps to shape these desires through the ways it creates products and markets them. Don't expect the Rudd Government to take on agribusiness in Australia, corporate food or the subsidies to these industries in consumer capitalism.
However, the food movement is broader than this, as evidenced in the slow food movement and farmers markets. Janet Flammang in The Taste for Civilization: Food, Politics, and Civil Society indicates a wider conception of the politics of food:
Significant social and political costs have resulted from fast food and convenience foods, grazing and snacking instead of sitting down for leisurely meals, watching television during mealtimes instead of conversingŌĆØŌĆö40 percent of Americans watch television during mealsŌĆöŌĆØviewing food as fuel rather than sustenance, discarding family recipes and foodways, and denying that eating has social and political dimensions.
The cultural contradictions of capitalismŌĆöits tendency to undermine the stabilizing social forms it depends onŌĆöare on vivid display at the modern American dinner table.
Posted by Gary Sauer-Thompson at 12:43 PM | Comments (5) | TrackBack
April 29, 2010
squeezing Big Tobacco
If the Rudd hospital reforms increasingly look as if they will make minimal difference to the way that public hospitals are run, then the shift to preventing smoking by ensuring that cigarettes would be sold in plain packs is to be welcomed.
This represents a reduction in cigarette advertising (brand names and product names will have to be displayed in standard colour, font style and position) and it will, according to leaks, be accompanied by a hike (25%) in the tobacco tax in the budget.

This public health policy is welcomed because it is a good public health measure: smoking kills people and the harm that it causes for smokers and non-smokers costs the nation around $31 billion.
The standard utilitarian argument is that if social costs are greater than social benefits then that activity should be taxed. Increased taxes act as a price signal to consumers to change their smoking habits. So Big Tobacco should pay some of the cost of smoking on the public health system.
Big Tobacco is outraged---the plain packaging legislation constitutes an expropriation of intellectual property rights (their trademarks). They are demanding billions of dollars to compensate for the loss of their trademarks. The argument is provided by Tim Wilson from the IPA in this paper on Intellectual property in a knowledge economy.
Commenting on this public health policy initiative Sinclair Davidson at Catallaxy says that Tobacco persecution continues. He says that both the increase in the tobacco excise and the plain packaging legislation are irresponsible and short-sighted.
However, in the latter Taxing fags: Repost at Catallaxy Davidson says that:
It is true that smoking has adverse health effects on smokers and non-smokers. This is well-known and has broad acceptance and understanding in the community and the incidence of smoking in the community has fallen dramatically in recent years.
So how does preventing people from dying from cancer square with the persecution of Big Tobacco? The latter implies a defence of Big Tobacco, the former implies the need to reduce smoking to prevent carcinogens.
So how do the right-of-centre libertarians square their circle?
Posted by Gary Sauer-Thompson at 10:48 AM | Comments (13) | TrackBack
April 19, 2010
CoAG: health reform
Today is crunch time to address the rapidly rising costs and inefficiencies in the fractured healthcare system at CoAG in Canberra. The common ground is that the system does need more money now rather than in 2014, and the commonwealth's contribution has gone down and down and down over the last decade. But extra funding does not necessarily mean higher quality health care.

Will the states accept the Commonwealth's bribes or sweetners and sign up to a limited public hospital program? Or will they---WA, Victoria and possibly NSW --- continue to resist signing over a portion of their GST, even though they tacitly agree that a single funder of health is best? That would begin to end the cost-shifting and finger-pointing that bedevils the current split system.
Or will they refuse to cut a deal and go out on a limb, even though the states have little hope of funding or supplying on their own the 21st-century system that we will need to deal with chronic illnesses and an ageing population over the next decade. And the states know it.
What we have, as Ian Hickie observes in the National Times is that:
The big dollars have been allocated to public hospitals and purchasing of elective surgery from the private sector. The real service commitments, particularly the guarantee that you will be treated within four hours of presenting to an emergency department, are clearly focused on improving the acute care sector only.
Nor are the states pushing for the rapid introduction of e-health despite the cost savings, or addressing the perverse incentives such as fee-for-service associated with bulk-billing in which clinicians are rewarded by the number of transactions rather than health outcomes.
Unsurprisingly, the states have been more interested in extra cash rather than addressing the underinvestment in prevention, early intervention and alternative care settings, particularly for older people. Lowering obesity rates, particularly among young people and those on lower income, or dental care do not seem to be very high on any real health priorities list. Nor is mental health.
Tony Abbott has little to say apart from it being another example of Rudd's smoke and mirrors. Peter Dutton, the Coalition's shadow health spokesperson, has nothing to say, as usual. No doubt they will oppose.
Update
The talks move very slowly---"inch by inch"--- by all accounts. Everybody has stayed on message about CoAG being constructive and everybody being willing to negotiate. NSW Premier Kristina Keneally has agreed to hand back 30 per cent of its GST to Canberra to help fund Kevin Rudd's hospital reforms.The commonwealth's claw back of GST to fund health care is the key sticking point, or bone of contention for Victoria and Western Australia. That issue has yet to be discussed at CoAG. Will it be debated tomorrow?
The Commonwealth continues to throw money around --this time it is $1.2 billion to help meet the emergency department and elective surgery targets set up under the Rudd's reforms. They are not talking about reducing the number of patients coming into hospitals through good primary care as David Burchell observes:
Unravel the righteous words about the importance of primary and community care, and it becomes clear that nothing much is about to change there, either. There are no specific proposals about nurturing "wellness", or better treating the epidemic of breast cancers, or dealing with mental health more effectively. Nor is there any evident revision of the received view that treats old age as if it were a form of illness, so that the elderly are condemned to spending their autumn years under the cold fluorescent lighting of hospital waiting rooms.The federal proposals won't make the business of hospitals easier, by keeping people out of them. They won't make the system fairer in any discernible way; nor, so far we can be told, will they work to restrain overall costs.
CoAG has yet to begin to seriously discuss health reform. What we have on display this time is more political posturing and positioning for upcoming elections.
Update 2
So it cost the Commonwealth $5 billion in incentives (including $1.2 billion to help meet the emergency department and elective surgery; $800 million for improved mental health services and 1300 extra hospital beds) to get the states on board plus a partnership with the states, with each contributing to a joint pool to fund hospital reform.
So the Commonwealth had to back down on directly funding the local hospital networks as the states are still involved in controlling the money. That state involvement through a joint funding arrangement to deliver hospital funding reform does mean the continuation of centralised and bureaucratic approach rather than giving the hospital networks the ability through direct funding to deliver locally crafted services according to the needs of the population.
Posted by Gary Sauer-Thompson at 7:29 AM | Comments (25) | TrackBack
April 14, 2010
Brumby = anti-reform
John Brumby, the Victorian Premier, increasingly stands for the self-interest of Victoria at the expense of Australia's national interest. He sabotaged water reform in the Murray-Darling Basin to keep water for Victoria with his anti-competitive, distortionary 4% trading cap--Rudd caved in and rewarded Brumby's intransigence, giving him substantial extra funding for water irrigation infrastructure in exchange for a vague commitment to remove the 4% water trading cap sometime in the distant future. Now Brumby looks as if he will play the same game around health reform with his intransigence and horse trading.
Brumby, it would seem, wants to lock in commonwealth money for the extra demand for health care to supplement his health budget, but without any strings attached. It is state rights not patient rights for Brumby. He stands alone in resisting health reform with his own plan Victoria, it seems, demands bribes (CoAG sweeteners) well beyond what the other states are receiving in order to sign up.

The health reform debate is focused upon issues of short run funding and the promise ofefficiency gains.If Brumby is now the arch opponent of the Rudd hospital reform plan, he does have a point this fight is about funding. The public hospitals' major problems are not about efficiency or management; they are about facilities and money, as a result of the Howard Government pulling money out of the system in the name of privatised medicine in the last decade.
As John Debble points out the Rudd Government is:
simply rebadging the part of the GST money the states and territories now spend on health as Commonwealth payments. About two-thirds would relate to hospitals. The other third would be the Commonwealth fully funding primary health services provided by the states, and there is a case for some adjustment
Moreover, the extra money over the next decade is simply the extra amount the Commonwealth would have to pay to maintain the average 8 per cent a year increase in state and territory health spending over the past 10 years.
State Premiers, such as SA's Mike Rann talk in terms of using these reforms to break the current log jam in healthcare to lock in partnerships between the commonwealth and the states; but the political reality is that the trajectory is one of increasing Commonwealth domination of the health sector. Is that a concern?
Now Brumby does not argue that we should work out the best way of providing health services, reforming the patchwork delivery system, and adjusting taxes to support the more effective delivery of better health services. Nor does he identify that drivers that would make the patchwork health systems improve and deliver what we want. These reform concerns are largely ignored. Brumby wants more commonwealth money for Victoria with no strings attached.
Posted by Gary Sauer-Thompson at 8:41 AM | Comments (9) | TrackBack
April 8, 2010
hospital reform: local governance
Health reform proceeds slowly. There is little movement towards health reform being less hospital-centric and more focused on the provision of community-based and preventative care or substantial mental health reform. Hospitals are places where people only need to be because of acute clinical danger (e.g. in trauma and psychiatry), or where rapid assessment requires investigations of the highest technology.
Australia still does not have a comprehensive platform on which to build community-based health services, as the brief flirtation with a nationally mandated community health program initiated in the early 70s was undone by subsequent governments.

The health debate is still about hospitals and it is mostly about the politics of health. Victoria and Western Australia are resisting the Rudd Government's proposal for the Commonwealth to take 60 per cent control of hospital funding by taking it form GST revenue. The debate, or theatre, has been about funding, not the creation of local hospital networks or a shift to activity-based funding.
Little has been said about governance, even though both major parties have advocated a return to the idea of local decision-making for pubic hospitals. Philip Davies points out in The Brisbane Line the local governance works for how hospital services should be delivered:
Figuring out the mix of staff needed to run a hospital, establishing a positive workplace culture, hiring the right doctors and nurses, choosing the equipment they need to work efficiently, and deciding how much to pay them are all issues that a local board would be well-placed to make. Those are arguably the areas where innovation on the part of local boards could have the greatest positive impact on hospitalsŌĆÖ performance.
The aim here should be to free local managers and clinicians from oppressive centralised control and foster innovation in local service delivery. The downside of clinicians playing a key role in future hospital boards is that their professional interests may be at odds with those of the local community. We may have a conflict between the protecting the high incomes of specialists at the expense of the equitable provision of healthcare in a world of limited resources.
Consequently, planning should be done at a state level. Davies says:
Individual hospitalsŌĆÖ roles need to be clearly defined and to fit together to form a coherent whole. Decisions about the location of costly, specialised services cannot be left to local hospital boards, however well informed or well-intentioned they might be. Difficult questions of resource allocation and prioritisation (ŌĆśrationingŌĆÖ if you prefer) are a necessary part of planning health care which we would delegate to non-elected bodies at our peril.
There is a role for government to set standards, allocate resources, define priorities and ensure coherence in services.
Posted by Gary Sauer-Thompson at 3:53 PM | Comments (7) | TrackBack
March 23, 2010
the politics of health
A health debate will take place between Rudd and Abbott today at the National Press Club, and it will be broadcast on national free-to-air television and Sky. The Canberra Press Gallery is delighted. More grist for their standard political frame of a Rudd v Abbott contest and they hope that there will be fireworks so they have something to write about other than who won.
So far it it has been less of a debate about health and more of a debate about public hospitals and the states. Rudd has provided increased funding for the hospitals, proposes to link the hospitals into local area networks and to fund them by taking 60% of the GST revenue from the states and introduce casemix hospital funding. Abbott's policy is local control of hospitals, more beds and, probably, federal funding for the local hospital boards.
So the "health " debate has been about who runs/funds the hospital system: the states, the commonwealth government, or local communities. It is hospital centric (more beds etc) despite the importance of community based services for mental health and aged care. Hospital centric is also how the Canberra Press Gallery frame the health debate.

What is not being addressed in the policy debate is the issue of how do we keep people health and out of hospital in the first place. These would include initiatives that will contribute to the prevention of chronic disease; better integrated, more flexible and comprehensive primary healthcare services; initiatives to enable health consumers to become better informed about how to stay or become healthy; integration of mental health into heal care and the modernization of health work force roles.
It is unlikely that these issues will be considered in the " great health debate" since Abbott is primarily interested in scoring points off Rudd---Rudd a policy ''fraud, fake and phoney'' etc -- than exploring how to address largely preventable chronic diseases associated with smoking, obesity and alcohol abuse ŌĆō diseases such as cancer, heart disease, stroke, diabetes and kidney disease.
Posted by Gary Sauer-Thompson at 8:56 AM | Comments (12) | TrackBack
March 22, 2010
paying nurses to play doctor?
Jeremy Sammut from the Centre for Independent Studies is a long term critic of the central thrust of health reforms under the Rudd Government towards prevention and primary care. He's a hospitals man. Health is about hospitals and acute care, not prevention.
His political philosophy contests the view that the state has a particular duty to help people lead a healthy life and to reduce inequalities. Sammut argues that the great lesson of the 20th century is that central-plan bureaucracies defeat any attempt at reform and streamlining. The only way is to replace them with independent, competing producers. This means freeing local hospitals from the stifling sameness of bureaucratic interference and mobilising the power of grass-roots problem solvers, with the hospital boards being held financially accountable for performance, as well as directly responsible to local communities.
So it is no surprise to find Sammut arguing against nurse practitioners being allowed to bill the Medical Benefits Scheme for treating patients with minor illnesses and prescribe certain medications on the Pharmaceutical Benefits Scheme in The Australian.
The basic argument is that spending too much money on treating the 'worried well' rather than patients who are actually sick--someone who spends years being treated for high blood pressure and high cholesterol - only to die of a rapidly invasive thyroid cancer. He says:
what Medicare has produced is an irrational and immoral rationing in the form of an inverse care law. People with no or relatively minor health problems can see the doctor free of charge and virtually on demand an unlimited number of times at taxpayersŌĆÖ expense, while people with serious illnesses are denied timely access to care and are forced to wait and suffer in the long queues for essential treatment in overcrowded hospitals. Paying nurses to substitute for doctors so the ŌĆśworried wellŌĆÖ donŌĆÖt have to wait is the wrong priority. This will simply pour more money into the part of the system that will do the least to improve health.
He adds that paying nurses to play doctor will see taxpayers money subsidise a new class of health entrepreneurs. It will not do what all good health reform should promote: the efficient use of scarce resources to ensure the truly sick receive better care.
Sammut's concept of the ŌĆśworried wellŌĆÖ---ie., people with no or relatively minor health problems---- ignores that with an ageing population and the increased prevalence of lifestyle diseases, preventing illness and keeping people healthy is Australia's best long-term insurance policy for the nation's health and managing the financial challenges ahead. Instead he says that:
the nurses union has flexed its considerable political muscle and convinced the government to use taxpayersŌĆÖ money to pay nurses to do the kind of community-based clinical work that many university-trained nurses now prefer to do.
This political argument ignores the argument that the prevention of chronic diseases argument: that good nutrition, exercise, and maintaining a healthy weight and regular health screenings for high blood pressure and high cholesterol can reduce the risk of stroke and heart disease. Healthy lifestyles may prevent a large proportion of mortality from chronic diseases in that they aim at modifying the conditions that make disease possible, or likely.
The 'worried well' scenario with its implication of disease mongering ignores the argument that, as the burden of chronic diseases increases, and as societal expectations in terms of quality of life and longevity also increase, prevention may offer an increasingly valuable alternative to treatment--- a focus on prevention rather than cure.
Posted by Gary Sauer-Thompson at 12:38 PM | Comments (12) | TrackBack
March 21, 2010
Obama + health reform
The House of Representatives in the US is expected to cast its final votes on health care reform in the next few days. It is considered to be the most important piece of domestic health legislation since the enactment of Medicare in 1965, and it is really needed.
Michael Tomasky has an interesting article on the impediments to health reform in the US in the New York Review of Books entitled The Money Fighting Health Care Reform. It makes for depressing reading as it shows how big money has increasingly dominated politics from the 1980s on. The result is that Congress has not passed a piece of major progressive social legislation for many years and a question mark is placed over whether Congress is capable of passing major, progressive domestic legislation anymore.
Tomasky says that on the big health reform question, the private health insurers won: if a health care bill is passed, it would contain no public option, no federal alternative that might compete with them.
The bill is still progressive in that it is fundamentally, an effort to address the the plight of the nation's 50 million uninsured. Ezra Klein says:
Once it's up and running, it spends $200 billion a year to help low-income and working-class Americans afford health-care coverage. About 15 million of those people will become eligible for Medicaid, which is public insurance. Another 15 or so million will get private insurance.
Tomasky does qualify his judgment that the institutional pressures of big money have effectively and quietly deformed central parts of the bill and continue to loom over any attempt by Congress to write and pass major domestic legislation. He says:
In fairness, the bill's many positive features should be recognized. It ends discrimination based on preexisting conditions and development of catastrophic illnesses. It eliminates price discrimination based on health status and offers subsidies for up to 30 million currently uninsured people. It establishes a host of other precedents concerning cost control and new services that would, taken together, still be a major, even astonishing, step forward. As big a victory as that would be, it will remain the case that it could have been a considerably better bill, in both providing medical care and controlling costs.
The bill would significantly change the way healthcare is paid for and delivered in the United States, and it would represent an enormous expansion of access to medical care for those who are uninsured or under-insured.
Update
It does look as if the Democrats will have the votes they need to pass the health reform bill. Obama has spent political capital, trading popularity for health care reform, and has succeeded by the narrowest of margins. Obama is now one of the handful of presidents who found a way to reshape the nationŌĆÖs social welfare system.
The Republicans strategy was to throw everything into killing the bill instead of working with it, and to hope that this would result in the bill's defeat. The entire strategy was predicated on killing the bill by arguing that big government was intruding into the lives of citizens.The bill is now passed, and it means that the US health care system has been fundamentally changed, and there will not be the votes to repeal it. The Republicans echo chamber is now talking about the healthcare wars.
Posted by Gary Sauer-Thompson at 3:00 PM | Comments (8) | TrackBack
March 11, 2010
health debate: #2
As noted in an earlier post, the health reform debate in Australia takes place behind a closed shop and it needs to be bought out into the public sphere. Arthur Sinodinos in his King Kong health plan threatens the PM in The Australian says that:
Health and hospitals policy is Kevin Rudd's King Kong and it could cause him as much damage as Kong did to the Empire State Building... These complex health changes will be a slow burn politically. The electorate has at least six months to pore over them and uncover any defects. The dearth of new money up-front will not help the medicine go down. When does the system start to improve? Paradise postponed yet again.
He contrasts this scenario with the good things the Howard Government did for health ---adding significantly to Medicare, particularly through its extension of the safety net--- and rescuing private health insurance. Sinodinos is contesting the view that health is Labor's home ground.
Subsidizing private health insurance is a classic example of the neo-liberal policy of the diverting of public funds to private industry, but Sinodinos talks in terms of "choice". Patrick Brownlee in Politics is a messyanic business in the Australian Review of Public Affairs digs beneath "choice" between public and private sectors. He says that subsidisation of private health (and education) should be recognised as part of the desiccation of the social contract that is transforming a collectivist to an individual incentive model of service delivery and created or pandered to a faux middle class sensibility.
Brownlee adds that:
The privatisation of education and health are dear to a neoliberal heart, where quality service is provided to those who have; while the idea that funds be collectively held and distributed by government for any such service causes at least mild reflux in your average neoliberal stomach.
Neoliberalism is a political ideology which extends market relations into social, economic and political spheres and it represents governance through the market.
Posted by Gary Sauer-Thompson at 8:53 AM | Comments (2) | TrackBack
March 9, 2010
the health debate
The health debate has been dominated by the media reducing health and well-being to hospitals and the state's resistance to the Rudd Government's reforms in the form of taking control of the funding of public hospitals. Their concern is for more money not that hospital care is integrated with primary care. John Menadue in his comments on this debate at the Centre for Policy Development that:
The [commonwealth] government is challenging, quite correctly, the special interests of state governments and their health bureaucracies. What is needed next is for the government to find the political will to challenge other stronger special interest groups, particularly among the providers - the AMA, the Australian Pharmacy Guild, pharmacy companies and the private health insurance funds. They have legions of lobbyists who dominate the public debate at the expense of a community that is effectively excluded and disenfranchised.
The current debate is still between the government (commonwealth and state) and the well-funded and well-organised special interest groups, and the community and its concerns is pushed aside.

Menadue's solution to the closed shop that excludes the community is for our health system to have its own independent body - a Reserve Bank for health--- an independent health commission with strong economic capabilities is necessary to facilitate informed public discussion, counter the power of special interests and determine programs and distribute Commonwealth health funds across the country.
Posted by Gary Sauer-Thompson at 8:45 AM | Comments (4) | TrackBack
March 4, 2010
local control of health
The authors of Putting Health in Local Hands at the Centre for Policy Development rightly argue that the health care system is more fragmented and duplicative, inequitable and less efficient than it might be.
They then suggest that "shifting health care governance and funding to regional agencies that are more responsive to the needs of communities would improve both equity and effectiveness in Australian health care."

They propose that all current health care funding from local, state and federal governments be pooled within a national agency and equitably distributed to local Regional Health Organisations (RHOs ) on the basis of evidence about health care needs.
They argue that the current emphasis on hospital care, rather than primary and preventive care, is increasingly recognised as inefficient and that there is broad agreement that effective primary care reduces health care costs and that improved access to primary health care services in the community would reduce unnecessary admissions to hospitals. However, our current system of primary care does not deal well with chronic diseases, nor does it work effectively with the acute sector.
To achieve more efficient and equitable outcomes it is not enough simply to shift resources from hospitals to health centres; we must address the social determinants of health and the inequalities of health in that the rich, urban, and healthy access more health care resources and services than the poor, rural, and sick.
Posted by Gary Sauer-Thompson at 5:06 PM | Comments (4) | TrackBack
March 3, 2010
finally, some movement on health reform
I see that Rudd has agreed with the common criticism of his government:--that the government has not progressed enough on delivering on its promises and Labor has not managed its issues - in particular the emissions trading scheme - effectively. Acknowledgment and acceptance of criticism is the first step.
Is it a tactical move---a circuit-breaker? Maybe. Maybe not. Stephen Leeder gives Rudd credit.
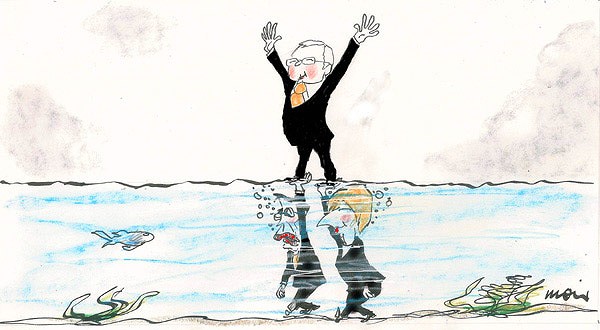
At least the criticism has resulted in steps taken towards health reform--- to get back to shaping the political agenda again shift. The reforms aim to shift away from Australia's heavy dependency on hospitals; to establish a new "independent umpire" at arm's lengths from government; to set "efficient national prices" of health services to be paid for by federal and state governments; the federal government taking over full funding responsibility for primary health care outside the hospital system; and new "Local Hospital Networks" paying for services, replacing the traditional model of Commonwealth grants to the states and territories.
An optimistic interpretation is that the Rudd Government is seeking to reduce not increase use of public hospitals, thus easing the strain, by putting in place a more efficient, integrated arrangement which, it is hoped, will spur people to be treated by less expensive primary health, (ie outside hospital) services.
However, what has been tabled in the reform agenda is two systems of government talking to one another with the commonwealth saying its gonna be xyz. Will the states concur? Will they reject it? No doubt more bribes (extra money as bait says Michelle Grattan) will be required to get them to accept national performance standards and the historic shift of power to Canberra on health care.
Update
I've re-read Rudd's Better health, better hospitals speech more closely. The core emphasis is that this fundamental reform is about improving hospitals. Rudd says this is:
Reform that for the first time enables eight state-run systems to become part of a single national network, using consistent national standards to drive and deliver better hospital services. Funded nationally. Run locally.The National Health and Hospitals Network contains seven major reforms. For the first time, the Australian Government will take on the dominant funding responsibility for all Australia's public hospitals from the states because the states simply cannot afford to fund the future growth of the system.
The Australian Government's funding share will almost double, from 35 per cent today to 60 per cent into the future - equating to an additional $11 billion per year from next year.The Australian Government will take clear financial leadership in the hospital system, permanently funding 60 per cent of the efficient price of every public hospital service provided to public patients.We will fund 60 per cent of recurrent expenditure on research and training functions undertaken in public hospitals.We will fund 60 per cent of capital expenditure - both operating and planned new capital investment - to maintain and improve public hospital infrastructure.
No previous Australian Government has accepted any responsibility for the funding of hospital infrastructure - let alone 60 per cent.Over time, we will also pay up to 100 per cent of the efficient price of 'primary care equivalent' outpatient services provided to public hospital patients.These reforms will permanently reverse the decline in the Australian Government funding contribution for public hospital services over the last decade.They will put an end to the tiresome cycle of the blame game between the Australian Government and the states over hospital funding.
There really wasn't that much on primary care and nothing about health inequalities. During questions after the speech Rudd suggested that itŌĆÖs hard for governments to invest in prevention because the benefits wonŌĆÖt be seen for 10 years or more. Therein lies the limits of this fundamental reform.
Posted by Gary Sauer-Thompson at 5:51 PM | Comments (17) | TrackBack
February 22, 2010
Sweet on health reform
Melissa Sweet makes a good point in her Intensive glare article in Unleashed about debates over health policy in Australia. She says:
in Australia we are stuck with a health debate that just cannot budge beyond hospitals, and Mr Abbott's headline-grabbing policy pitch for local boards to run hospitals simply reinforces that unhealthy focus.His plan creates yet another mechanism for focusing health funding and policies on institutions rather than on better meeting the community's health needs. It also provides another mechanism for enhancing division both between hospitals themselves, and between hospitals and the rest of the health sector, and for ensuring that health services remain centred around the needs of professionals rather than the community.
Health reform in Australia is still being reduced to talking about hospitals and doctors. If it is not about that, then it is about private health insurance industry. Most governments in Australia have avoided questions that involve confronting powerful vested interests in that industry
Posted by Gary Sauer-Thompson at 8:05 PM | TrackBack
January 8, 2010
the medical gaze
Though the concept of Medicalization needs to be revised to one over-medicalization, we still have the pharmaceutical industry busily engaged in shunting everyday problems into the domain of professional biomedicine.

This medicalization of the social is happening at a time of the erosion of medical authority; health policy shifting from access to cost control; managed care becoming central; the emergence of corporatised medicine; genetics becoming the cutting edge of medical knowledge and moving to the centre of medical and public discourse about illness and health; and the development of medical markets (cosmetic surgery).
Many socially unacceptable behaviors have been medicalized and assigned disease terms in the 20th century and we have the medicalization of depression in which the natural emotions of sadness are medicalized as a depressive disorder.
These are examples of the way that medicine as a dominant institution has expanded its gaze in the past half century or more and become central to the subjectivities of people's lives. The mechanisms here are both the transformation of the normal (sadness) into the pathological (a depressive disorder) and the way that medical ideologies, interventions and therapies have reset and controlled the borders of acceptable behaviour (social deviance), bodies (overweightness ) and states of being (social anxiety).
Over medicalization is now a common part of our professional, consumer and market culture in a post Prozac world--eg., medicalizing aging bodies (both female and male) in an attempt to control old age. This medical market is about pharmaceutical companies constructing and marketing diseases (anxiety) and then selling drugs (Paxil) to treat those diseases.
Another example is testosterone therapy for the treatment of male menopause (running on empty) to restore or enhance masculinity that plays withe body-as-machine metaphor. Men can fill up the tank with drugs to regain their sex drive, energy and optimism to become the sleek, powerful machine they desire to be.
Posted by Gary Sauer-Thompson at 11:42 AM | Comments (3) | TrackBack
December 9, 2009
Medicare Select
In its final report to Government, the National Health and Hospitals Reform Commission introduced the idea of Medicare Select. It represents the introduction of a market mechanism (managed competition) into Medicare without embracing the free market attack on Medicare by market economists and the private insurance health industry in order to introduce a for-profit model that would be driven by the insurance industry.
The purpose is to slow growth in health expenditure, a key or core policy issue for state and commonwealth governments, by introducing a degree of self-regulating capacity within health care systems. Richard Scotton argues that:
The managed competition model offers a framework within which the objective of increased efficiency could be pursued without sacrificing the goal of universal access and without the impairment of health outcomes and social cohesion which the abandonment of this access would involve.
Medicare Select is a universal, tax-funded health insurance scheme based around the purchaser-provider distinction.
It formed part of the National Health and Hospitals Reform Commission's proposal to move towards a single government funder across the care continuum ŌĆō both inside and outside hospitals .The ŌĆśMedicare SelectŌĆÖ model suggests a transition of the commonwealth government from a funder of services to a purchaser of services.This involves the separation of the government from the functions of the organization and management of care consumption (eg.,explicit rationing of services) and the provision of care or health services. These functions would generally be undertaken by different organisations.
Who then provides the health or care services? Those called 'budget holders'. These would mostly be existing private health insurance funds. Consequently, Medicare Select represents the expansion of the private sector in health care, and it is likely that managed care would be used as a tool in managed competition.
The Parliamentary Library describes this scheme thus:
Under Medicare Select, the Commonwealth Government would become the sole public funder of health services. It would then distribute funds to intermediary bodies called ŌĆśhealth and hospital plansŌĆÖ. The government would operate at least one plan, which would compete on equal footing with plans operated by not-for-profit or for-profit organisations.By establishing these plans, the Commonwealth Government would separate the funding or purchasing functions in health care from service provision. Economists refer to this as a ŌĆśpurchaser-provider splitŌĆÖ and many suggest that it increases efficiency, largely because single funders tend to have lower administration costs and substantial power in negotiations with providers.
Under Medicare Select, membership of a plan would be compulsory thereby ensuring universal access to basic health services. All people would initially be members of a government operated plan but would be free to choose another one after the scheme began. Plans would be required to accept anyone who wished to enrol. There would probably be some restrictions on when and how people could change plans, as there are in other countries with similar systems.
Posted by Gary Sauer-Thompson at 7:21 AM | Comments (3) | TrackBack
December 8, 2009
Open Government + health reform
The Draft Report of the Government 2.0 Taskforce has been released. It makes interesting reading in the light of CoAG stalling on health reform yet again by stating that it will take 3 years to produce a a health reform plan. This reform promises to deliver a new era of federal-state cooperation and to end the buck-passing and blame shifting that has characterised past state-federal relations.
The public service culture is one of secrecy and it instinctively resists becoming more open and transparent by releasing much of the information now kept secret. Reform here means a pro-disclosure culture. So what have the public servants been doing in crafting a response to the National Health and Hospitals Health Reform Commission's report, the draft National Primary Care Strategy, and the National Preventative Health Strategy
The Rudd Government basically accepts these reports. Where are the background papers that the public service has used to craft the government's response to these reports? Is there any indication of greater information disclosure, digital innovation and online engagement?
CoAG gives very little away in terms of openness and transparency. All we know is that state and federal leaders have agreed to work towards developing specific proposals in the first half of next year:
The Prime Minister will correspond with First Ministers by the end of December 2009 recommending a decision-making process on long-term health and hospital reform. In this process the Commonwealth will actively engage with the States on the range of reform proposals canvassed by the National Health and Hospitals Reform Commission and related proposals. The CommonwealthŌĆÖs intention consistent with this process would be to put specific proposals to the States in the first half of 2010.
Which specific proposals are these? What are the arguments from the working groups? What are the working groups and what are they working on? What is the best available option, taking into account the current and future needs of the Australian community and the political and practical realities of implementing reforms?
We have no idea. The public service culture is one of secrecy not open access government, and the steps being taken to becoming more open and transparent are minimal. Federal and state bureaucrats talk to one another. The powerful lobby groups use their resources to gain insiders information and shape the discussions to protect their interests by blocking reform. Governments, even when in favour of public innovation, are not really comfortable being open with their inner workings on display. As Michael Richardson points out:
Openness can make life tough. Transparency opens the door to criticism; ending secrecy increases risk and exposure; accountability means being held accountable.
It is true that the old ways die hard within government and especially in health, which is run by medical experts within a heavily walled insider culture, despite the overarching policies of openness and transparency, the embrace of Web 2.0 by some government agencies, and the public interest in the quality and safety of our hospitals.
However, as Jennifer Doggett points out at Croakey the Rudd Government spent two years wooing health groups with promises of a partnership approach to restructuring the health system, then COAG has reneged on its obligations at the last minute.
The medical culture, deliberative democracy and Web 2. 0 just don't mix. What we have is the AMA, an anti-reform body, posing as the advocates for health workforce reform According to Melissa Sweet. at Croakey the spin from the AMA is one of:
the AMA as the advocate for health workforce reform, including using nurse practitioners to help alleviate workforce shortages. The AMA advocating for the end of the private health insurance incentives which have helped entrench the unfairness of our health system. The AMA advocating for a rebalancing of power within the profession and its structures, to give supremacy to the primary care end of town. The AMA advocating for doctors to work in areas of need, rather than in areas of comfortŌĆ”
Web 2.0, plus openness and transparency, would help to break the stranglehold the AMA has over health policy and provide a space for other voices.
Posted by Gary Sauer-Thompson at 9:10 AM | TrackBack
November 26, 2009
Open Australia
I've been interested in the ideas surrounding, or flowing from, Government 2.0. One of these was Mashup Australia, which was designed to provide a practical demonstration of the benefits that open access to public sector information can provide. I've been curious about how this could help improve my blogging by providing me with greater information.
One example of the potential that can be unlocked when government information is unlocked by pulling together data sets in new and innovative ways is Open Australia, which I stumbled upon yesterday. This is a volunteer run website that helps us to find out what our representatives are getting up to in parliament with the aim of bridging the growing democratic disconnect or deficit that many people feel.
It was always difficult for those outside Parliament to follow debates in Parliament on any issue as it involved scrolling through pages of Hansard record of the day (a pdf) to find the issue. It was too unstructured. The other option, of listening to Senate debates online via a live stream is particularly tedious, especially when the speakers are a bunch of climate change denialists.
Thus we have Senator 'free enterprise' Cory Bernadi's rhetoric about alarmists, leftists, the new religion of climate change, heretics and sceptics, political madness, OrwellŌĆÖs Big Brother, climate science as a fraud and so on and so on. I just stop listening This kind of content sees climate change through the left-right prism of the culture wars, junk science and delusion in the sense of turning away from reality.
It can be found in the op-eds of Miranda Devine whose wingnut rave is about the heart of the propaganda machine of climate science that has driven the world to the brink of insanity; climate alarmists are dangerous megalomaniacs, foolish, but with enormous power. And so on.
So what does Senator Alan Ferguson, also from SA, who have to say by way of contribution to a public debate.
I am in a rather unique position, having started to make this speech last night prior to any knowledge of proposed amendments and, now, having seen those amendments, I can move on. Can I say first of all that seeing those amendments has not made me any happier. My opposition to these bills remains the same as it was. My position has not changed from last night now that I have actually seen the amendments.
No reason is given for this position. We are offered no argument as to why. It is just assumed that the dismissal of the McFarlane deal is reasonable without giving a reason. Exasperation is my response at the trashing of the values of democratic deliberation and debate.
Senator Concetta Fierravanti-Wells from NSW says:
what has troubled me about the current debate is the language and tone of the public utterances. On the one hand, there has been a fervent, almost evangelical, adherence to a view that the sky will fall in if the world does not act on climate change now. Advocates of this position have pilloried those who have dared oppose their view. They have dubbed them ŌĆśclimate change scepticsŌĆÖ in tones reminiscent of the Inquisition and burning people at the stake. Some have stridently and appallingly equated them to Holocaust deniers. YesterdayŌĆÖs front page article in the Australian, entitled ŌĆśHackers expose climate brawlŌĆÖ, and the release of emails only strengthen the views of those who have questioned the science. The apparent glee at the death of one such scientist by those holding opposing views is both sickening and appalling.On the other hand, people have questioned the science. We have seen scientists, such as Professor Plimer, offering alternative viewpoints.
After a while listening to this kind of rhetoric about science that makes a virtue of ignorance is just too much. I just switch off. Fierravanti-Wells is basically defending the coal interests in the Illawarra region. Ever more protection for the coal miners is her policy. This is the ground to fight an election on for the conservatives. They do not seem to realize that they would go backwards, or they don't care. It's a long term split.
Open Australia means that the information is now very easy for bloggers and citizens to access what is being said on particular debates by our local members or Senators inside Parliament. So were can see where they are coming from and how much they support a reform process. Thus Senator Birmingham from SA, in speaking on the Australian National Preventive Health Agency Bill 2009 makes the following observation says:
that no number of marketing campaigns, no number of budgets in these areas will enable you to convince or stop people from making what in the end to some extent are free choices to be able to actually decide how they lead their lives. Unhealthy lives we would all like to discourage, but there are limits to how much government should interfere in peopleŌĆÖs lives to discourage them from leading unhealthy lives. Government is not some nanny state that is there to hold the hand of everybody each time they go to the supermarket, to tell you, ŌĆśNo, you should not put that in your shopping trolley.ŌĆÖ That is not the role of government and that is not what we should be seeing out of these types of preventive health agendas.
Birmingham appears to accept that a preventive approach to sickness is fundamental to any good health system but is concerned that the debate has not actually focused on when we cross the line of unnecessarily telling people how they should live their lives.
As Pip Marlow points out:
the agenda of Gov 2.0, and of the whole project of providing transparency and openness in government data, cannot be met unless we deal with the challenge of finding the ŌĆ£jewelsŌĆØ, the ŌĆ£gemsŌĆØ in the unstructured data itself.
Open Australia makes it possible to access what our representatives are actually saying behind the spin of media releases, doorstops, and media interviews. We can access what hey are saying at work, so to speak.
Posted by Gary Sauer-Thompson at 7:32 AM | Comments (1) | TrackBack
November 3, 2009
supermarkets, food, health
Jon Wardle and Michael Baranovic conclude their article in the latest issue of The Brisbane Line by saying that:
Health problems are no longer being caused by lack of access to food but rather by lack of access to foods that provide the most health benefit. We need to look at food provision in a more integrated manner that extends beyond just price. Until the issue of a competitive fresh food retail sector is seen as a public health priority, the significant and entirely preventable impact of poor nutrition on health will remain a millstone on AustraliaŌĆÖs health policy.
Most of their article is about the lack of competition in the fresh food retail and grocery sector due to the dominance of the Woolworths/Coles duopoly in Australia and how to ensure healthier competitive practices.
What is assumed is that the food industry causes health problems, that a preventative health policy ensures an equitable access to healthy, nutritious food, and that there is a literacy amongst consumers about the importance of healthy food for their wellbeing.
What is not mentioned by Wardle and Baranovic is that in spite of the claim of selling fresh food the supermarket shelves are full of foods full of sugars, fats, refined starches, artificial sweeteners, preservatives, colours, flavours and other additives. As Rosemary Stanton observes in Crikey:
The vast array of foods ensures we over-eat. The average supermarket now stocks 1800 different snack food lines, more than 150 breakfast cereals (some more accurately described as confectionery), and an absurd choice of junk in aisles stocked with packet soups, sauces, biscuits and sugary drinks. Does it really make us happier or healthier to have 45 varieties of milk or hundreds of choices of yoghurt?.. there is an urgent need to reduce the national girth. The most popular call is for more physical activity. No one would argue with that. But we also need to find a way to encourage people to eat less.
And to encourage people to eat differently--to eat more fresh food rather than the junk foods that are high in saturated fat and sugar. Stanton adds that:
The usual cry of ŌĆ£they should be educatedŌĆØ doesnŌĆÖt work in the face of so much abundance and strong marketing campaigns to get us to eat more. Food industry profits depend on us eating more. The food industryŌĆÖs solution of more choice increases profits, but does nothing for obesity.
I am sure that the food and drinks industry will both actively lobby against the recommendations of the Preventative Health Taskforce that will impact of their profits; and reposition themselves as the true friends of public health and market themselves as selling healthy products.
No sales tax on sugary soft drinks and fatty foods would be one example that would not go down well the food industry. They would resist this for sure.
Posted by Gary Sauer-Thompson at 3:20 AM | Comments (21) | TrackBack
October 21, 2009
the nanny state
The Nanny State refers to state protectionism, economic interventionism, or regulatory policies (of economic, social or other nature), and the perception that these policies are becoming institutionalized as common practice. It is used to refer to the Rudd Government and it is argued that we liberal citizens should boldly resist this attempt to strangle our basic freedom.

Thus Julie Novak, a research fellow with the Institute of Public Affairs, says that the National Health Preventative Taskforce is proposing to use 'nudge' social arrangements to ensure that 2020 Australians should be beer-refusing, meat pie-avoiding non-smokers.
The 'nudging' is designed to stop us from eating, drinking and smoking anything the government disapproves of. The Rudd Government desires to control what we put into our bodies, and this statism stands for a "coercive utopia".
Novak acknowledges that preventative health arises because of the blowout of future health care costs to save lives and reduce health costs:
It is argued that governments need to get involved in people's consumption choices because of potential health problems that are borne by taxpayers through the health system....This argument runs the risk of degenerating into slippery slope arguments for even more prescriptive controls over individual choices. For example, should individuals not drive cars any more so that public hospitals do not bear the costs of treatment if car accidents befall them? The health system exists for people to use, and should be separated as far as possible from questions of individual choice.
This is misleading. The issue is about drinking and driving and causing harm to others. Secondly, it is liberals, horrified by the blowout of the health budget, who have proposed that individuals take responsibility for their ill health---eg., obesity. This self discipline is done to counter what they call an "entitlement mentality", by which is meant that individuals expect that governments will step in to fix any and all problems that may arise.
Novak's position is that our precious liberties (negative freedom) have to be left intact. So how does she propose to improve our health? She says that:
it can also be argued that there are more effective research paths to help improve our health and life expectancy.Think of the serious, cutting edge research and development into new drugs by pharmaceutical companies that often require billions of dollars but promise massive payoffs.
So she is effectively speaking for the drug companies and for a pharmaceutical approach to preventive health care. This approach to health care is not argued for.
Posted by Gary Sauer-Thompson at 10:11 PM | Comments (6) | TrackBack
October 18, 2009
flicking the switch away from vaudeville
In her Good policy wielded with a big stick op-ed in The Age Katharine Murphy makes a good point:
To borrow a famous Keatingism and adjust it for the times, in Canberra it is time to flick the switch away from vaudeville. It is time for hard policy decisions that will ultimately define the Government and its legacy.We have heard much rhetoric in recent months about the Government's ''productivity revolution''. Until very recently, your columnist had no idea what this might be, apart from spending on infrastructure (much of which state governments should be doing if they could run their finances properly) and some nascent policy work in the area of education.
Murphy goes on to talk about the productivity revolution in terms of the national broadband network (lower prices, better services, instant connectivity) and tax reform replacing Australia's inefficient system of road and petrol taxes with congestion charges.
What Murphy misses is the process of health reform under Rudd and Roxon, which is designed to increase productivity through healthy workers. Healthy workers are productive workers. Sick workers are unproductive.

Murphy's interpretation of the recent shift in health policy to primary care, lifestyle illness and preventative health is a libertarian one. She says:
The fat police are well intentioned and, no doubt, learned public health experts, who would like us to stop scoffing junk food and lolling on the couch.They would like to ban junk- food advertising because they would prefer it if kiddies ate carrot sticks and organic raisins, and went for brisk walks in the outdoors.The fat police would like it very much if we'd stop being fat .....Why is it - someone remind me please - that we want governments to do things?
Now there is some strange logic in this debate--eg. some argue that the state intervening to deliver health outcomes is ŌĆśnot political', whilst the state leaving individuals to make their own choices is ŌĆśpolitical'. However, the 'fat police' is misplaced since what is happening is that the mode of governance is shaping of the conduct of free subjects in the world of neo-liberal capitalism.
We have a bio-politics of the population that focuses on a series of interventions and regulatory controls of various aspects of human life such as birth, health, longevity, sex, and mortality coupled to modes of construction of neo-liberal subjects.
Posted by Gary Sauer-Thompson at 4:07 AM | Comments (2) | TrackBack
October 6, 2009
whither health reform?
Is the Rudd Government serious about health reform? By health reform I mean the need for increased investment in primary care. ThatŌĆÖs the key to improving health outcomes, access and equity. All the pictures on TV and the press have been about Rudd, Roxon and Elliot having consultations with health professionals in public hospitals. The message is that health equals hospitals.
Isn't that reduction what is supposedly being reformed? Do we interpret the meaning of these carefully prepared images as the Rudd Government is "in the process of retreat from any serious health reform? That health reform becomes the equivalent of sorting out the hospitals?
That is how I am reading the signs. This is what appears to be the case. I am prepared to concede that it may not be--that Rudd and Co will not promise heaps--a revolution ---then deliver very little.
The responses to the promised reforms to primary health care have been interesting. For instance the Institute of Public Affairs (IPA, has argued that the National Preventative Health TaskforceŌĆÖs report is more or less a grab for more bureaucratic power, and a grab for more tax by government, in that the TaskforceŌĆÖs report advocates widespread government interference and control over individual choices by the nanny state.
According to the IPA the Preventative Health Taskforce's report argues that people get fat because they eat too much and don't exercise enough. The taskforce's solution -- the government needs to make sure people eat less and exercise more. It is a government shove on how average Australians should live their lives:
the taskforce recommends imposing heavy sin taxes that will increase the price of food, alcohol and cigarettes. But these tax increases are unlikely to have any additional effect on existing taxes, advertising bans and horrific warning labels about the consequences of smoking. They are likely to act as a regressive imposition on the least well-to-do in our community. The only beneficiary is likely to be government coffers. Increasing taxes as a deterrent has a poor record of success.
Australians can make rational, informed decisions and still smoke, eat fast food and binge-drink beyond the technical standard of three glasses of booze without destroying our health, as long as we are encouraged to take responsibility for our lives and should accept the consequences. However, the government is removing choice from individuals and is creating a society where experts determine how we live our lives.
The debate takes place because few in public health think that an exclusive focus on individual food choice or personal responsibility is sufficient to combat the obesity epidemic, any more than it was to combat the epidemic of tobacco-related disease. It is akin to smoking, which was once seen as an individual choice and has has become a major public health issue with a high degree of regulation. Obesity is a political issue as well as a health issue. It is political because the debate is whether the government has a limited role or that it has a significant one.
Supporters of the first view insist that overweight and obesity result from daily lifestyle choices. They believe adults should not only make positive choices for themselves, but also supervise their children in terms of nutrition and physical activity. They feel the governmentŌĆÖs role is to provide health information and facilitate behavior changes through the support for education, research, and community-based interventions.
Proponents of a more active government role argue that overweight and obesity result from a complex interplay of behavioral, environmental, and genetic factors, and that the government needs to undertake broad policy initiatives ranging from regulating the food environment and prescribing physical activity and nutrition for children, to supporting urban planning for increased physical activity through transportation and public safety provisions.
The public health approach focuses on population rather than on the individual and it is highlights the power of the food lobby defending its interests, as Big Tobacco did with cigarettes when faced with evidence of tabacco as an addictive carcinogen. The problem of obesity has moved beyond an issue of individual choice to become a societal problem that requires public policy change
Posted by Gary Sauer-Thompson at 3:12 PM | Comments (4) | TrackBack
September 9, 2009
health reform: primary health care
Building a 21st Century Primary Health Care System says that it provides a road map to guide future policy and practice in primary; that represents the first comprehensive policy statement for primary health care in AustraliaŌĆÖs history; and presents the Australian GovernmentŌĆÖs views on possible future
directions for a modern 21st century primary health care system.
The right implication is that Australia has been until now, going along without any strategy or sense of direction. The draft strategy acknowledges the obvious: that the health system overall would benefit if a more systematic response from primary health care, together with more effective integration of other health sectors with primary health care, could be achieved and secondly, primary health care services have historically been delivered in a relatively unplanned environment.
Consequently, primary health care in Australia currently operates as a disparate set of services, rather than an integrated service system:
it is difficult for primary health care to respond effectively to changing pressures (such as demographic change, changes in the burden of disease, emerging technologies and changing clinical practice) and tocoordinate within and across the various elements of the broader health system to meet the needs of an individual patient.
The Strategy talks in terms of key building blocks (regional integration, Information and technology, including eHealth, skilled workforce, Infrastructure, and financing and system performance) and priority areas for change (improving access and reducing inequity, better management of chronic conditions, increasing the focus on prevention and improving quality, safety, performance and accountability).
Posted by Gary Sauer-Thompson at 11:53 AM | Comments (1) | TrackBack
August 25, 2009
Queensland: Abortion Law
Queensland is an odd place. It is the face of modern Australia as well as that of old Australia. QueenslandŌĆÖs abortion laws are now the most antiquated and repressive in the country. Abortion remains a criminal offence. As Professor Caroline de Costa has pointed out in Crikey:
Both medical and surgical abortion, even by registered medical practitioners, remain crimes in Queensland under legislation that uses wording from 1861...It is true that there have been no prosecutions of doctors since Dr Peter Bayliss was acquitted in 1986 but the law remains in the Criminal Code, and as the case currently before the courts in Cairns shows, the police are prepared to prosecute both a woman making a personal decision for herself, and her supportive partner.
Queensland women are now having to travel to Sydney for a medical abortion since the protection offered to doctors who perform abortions in Queensland, based on the case against Dr Harry Bayliss in 1986, only applies to surgically-induced abortions.
de Costa adds that so far the Bligh Government:
has suggested letters and words of reassurance for doctors, and some tinkering with section 282 of the Criminal Code so that there is a defence for medical as for surgical abortion. The assurances of persons currently in positions of power provides little legal certainty even while those people remain in their posts, and none whatever when they depart.
Premier Bligh did say on Q+ A that her personal view is that abortion should be a matter between a woman and her doctor. However, she quickly added, there shouldnŌĆÖt be any attempt to change the existing law because there wouldnŌĆÖt be the numbers in the Queensland Parliament for it to get through.
So there is to be no decriminalisation of abortion in Queensland under a Blight Government. Something needs to be done. As Andrew Bartlett points out the situation for individual women seeking an abortion and for doctors prepared to provide is now totally untenable. Beirne School of Law Associate Professor Heather Douglas at the University of Queensland said:
Studies suggest that around 80 percent of survey respondents agree that a woman should have the right to choose whether she has an abortion. For many women - and for the health budget- abortion using drugs is a safer and cheaper option. As a result of the current legal position, there is virtually no access to abortion through the public hospital system in Queensland. This means that abortion in Queensland is also a class issue. Women with greater access to funds are more able to travel to obtain an abortion and to pay the private medical fees associated with abortion.
The ethical point is that woman should never be prosecuted for undergoing abortion, that the decision about abortion should be between the woman and her practitioner; and the regulations covering abortion should be in the health regulations in the 21st century.
What now? Women should be able to access safe legal abortion and should not have to suffer further indignities and possible penalties because she has sought and had an abortion performed.
Posted by Gary Sauer-Thompson at 2:55 PM | Comments (10) | TrackBack
August 23, 2009
backlash against Obama
In his ObamaŌĆÖs Trust Problem in The New York Times Paul Krugman refers to news reports that the Obama administration ŌĆö which seems to be backing away from the ŌĆ£public optionŌĆØ for health insurance ŌĆö is shocked and surprised at the furious reaction from progressives. Krugman adds:
A backlash in the progressive base ŌĆö which pushed President Obama over the top in the Democratic primary and played a major role in his general election victory ŌĆö has been building for months. The fight over the public option involves real policy substance, but itŌĆÖs also a proxy for broader questions about the presidentŌĆÖs priorities and overall approach.
Progressives are now in revolt. Obama took their trust for granted, and in the process lost it. And now he needs to win it back. Krugman's argument here is similar to what is happening in Australia. There the Rudd Government is losing the trust of progressives due to its very watered down climate change policy, priorities and overall approach to energy.
Krugman's argument is part of an ongoing debate in the US about the politics of health care. "Change" is what Obama stood for. "We can do it" Change sure was needed in health care.
Glenn Greenward says that:
The central pledges of the Obama campaign were less about specific policy positions and much more about changing the way Washington works -- to liberate political outcomes from the dictates of corporate interests; to ensure vast new levels of transparency in government; to separate our national security and terrorism approaches from the politics of fear. With some mild exceptions, those have been repeatedly violated. Negotiating his health care reform plan in total secrecy and converting it into a gigantic gift to the pharmaceutical and insurance industries -- which is exactly what a plan with (1) mandates, (2) no public option and (3) a ban on bulk negotiations for drug prices would be -- would constitute yet another core violation of those commitments, yet another bolstering (a major one) of the very power dynamic he vowed to subvert.
Obama does need to toughen up given that the standard practice of the private medical insurance companies in the US is to kick people off their coverage when they get sick; to deny coverage to people who have previously been sick; to hide lifetime limits in the fine print, force people into bankruptcy if they face a serious illness; and to discriminate against pregnant women and their families. Their strategy is to squeeze every dollar they can out of patients in the current system, up until the last possible day they can.
Posted by Gary Sauer-Thompson at 2:10 PM | Comments (13) | TrackBack
August 20, 2009
Skeketee: the politics of health reform
Mike Steketee in Stumbling blocks on the journey to better health in The Australian highlights the key proposals of the National Health and Hospitals Reform Commission's final report. The recommendation is for the commonwealth to take full responsibility for primary healthcare, including presently shared responsibilities such as dental and aged care, as well as community services such as alcohol and drug treatment and mental health now run by the states.It suggests a shift away from fee-for-service medicine, which pays doctors for quantity rather than quality, to increased use of payments that reward outcomes or pay for the overall care for patients with chronic conditions.
Steketee argument is that though Kevin Rudd sounds deadly serious about wide-ranging reforms in health the question is whether the system, the politics and the economy will allow him to make them.
He does not sound like someone who has given up on health reform. But with the states already baulking over increased commonwealth responsibilities, it is hard to see how true health reform is compatible with the co-operative federalism in which Rudd has invested so much effort, unless a big commonwealth bribe to the states can do the trick.
Steketee adds that the National Health and Hospitals Reform Commission's final report caused relatively little offence, with a muted reaction so far from the AMA and supportive noises from the private health funds. That Rudd did not want the commission to look at the 30 per cent private insurance tax rebate helped with the politic.
Steketee's judgment is that the final report:
leaves an obvious gap: although the report dwells on growing pressures on health from increasing demand, technological advances and ageing, and says the system has reached a tipping point that requires tough decisions, it ignores the $4bn a year or more spent on subsidising private health insurance, the most inefficient use of government resources anywhere in health and an amount that would make a big difference if it were spent directly on hospitals, whether public or private. Talk about the elephant in the room.
We can put aside the rhetoric about "fundamental root and branch reform". This will be evolutionary change within political limits. of the possible.
Posted by Gary Sauer-Thompson at 12:37 PM | TrackBack
August 15, 2009
crazy people
If the antics we've seen over climate change and the CPRS is as loony as Australian politics gets, we should count ourselves lucky. Nothing we produce here can hold a candle to the American right. Nothing that wouldn't count as certifiable, anyway. They make Steve Fielding and Wilson Tuckey look like finishing school graduates.
Obama's proposed health care reforms have them in a frenzy, dragging the British NHS system into their personal debacle. It's been claimed that if Stephen Hawking had presented to the British system he would have been written off as a hopeless case and left to die. Never mind that it turned out Hawking is British and owes his life to the NHS, the scare is out.
There's talk of something they call 'death panels', whereby the elderly will be deemed expendable and given a nudge into the grave by government. Well, according to Sarah Palin, they will anyway. Sarah didn't make 'death panels' up all by herself. It's a leftover of the conservative arsenal against Clinton's health care reforms.
Another Republican meme doing the rounds escaped from a more friendly owner to end up plastered all over the American landscape in modified form.
Obama's not having much luck dealing with the lunacy. When town hall meetings organised to explain the scheme were hijacked by screaming loonies, the solution was to have Obama do a few, the idea being more or less 'look me in the eye and say that'. But when he tried, they didn't turn up.
Paul Krugman :
The truth is that the factors that made politics so ugly in the Clinton years ŌĆö the paranoia of a significant minority of Americans and the cynical willingness of leading Republicans to cater to that paranoia ŌĆö are as strong as ever. In fact, the situation may be even worse than it was in the 1990s because the collapse of the Bush administration has left the G.O.P. with no real leaders other than Rush Limbaugh.
He thinks there's no point carrying on the diplomatic approach with such people. Obama needs to simplify the message and drive it home. His commenters beg to differ. They say it's time to start pointing out what lunatics these birthers and tea party people really are.
In comments over at Club Troppo, Ken Lovell says:
Our Great and Powerful Friend, our ally and protector, has become a fractured and dysfunctional society that increasingly tries to promote and protect its self-identified global interests by the use of crude force. On any objective analysis it is a deeply disturbing situation that can only get worse. Yet hardly anybody wants to talk about it or even admit there is a problem.
Luckily our great and powerful friend can't inflict its fractured and dysfunctional health system on the rest of us, although its interests do attempt to burden us with its insane politics. This kind of stuff is bad for American society, and invariably works to the disadvantage of the crowds who tend to support it. But what's bad for them can be good for us. Watching both the antics and the state of the American health system, we can be grateful that Wilson Tuckey is as bad as it gets here, that at least Barnaby Joyce is funny, and that we know the benefits of Medicare.
Posted by Lyn Calcutt at 3:41 PM | Comments (9) | TrackBack
July 30, 2009
health reform: hospitals or primary care
A debate about health care is underway in Australia as a result of the National Health and Hospital Reform Commission's A healthier future for all Australians final report. It has organized its thinking around four issues: taking responsibility for health; connecting care; facing inequalities; and driving quality performance.
If the reform agenda is be a big part of the Rudd pitch for the 2010 election, then Ross Gittens warns that we should not expect too much from the Rudd Government, as it has a record of of over-promising and under-delivering. Our health culture is still one in which policies are driven by due process and authority and not by urgency or need.

Currently, the politics of health care is driven by access to hospitals----ie., waiting times for elective surgery and emergency services dominate discussion, the media and elections and ad hoc dabŌƤ reform aimed, , at one-off improvement rather than the creation of an adaptive, self correcting system, proactively seeking system improvement.
The ground is shifting. Even the AMA is acknowledging that general practice is not just about doctors any more. GPs, they say, must be supported by practice nurses, allied health and preventive health care providers to ensure we build on the strengths of AustraliaŌĆÖs primary care network and developing effective e-health systems. How both of these happen is a bone of contention. The common ground is that the one issue that offers the greatest promise for health care reform is connecting care more effectively and that it is primary health care and prevention that provides the pathway for the much better connection of care that is needed for consumers across programs, services and governments.
This common ground is contested by Jeremy Sammut, a research fellow at the Overcrowded hospital system needs structural reform to end bed crisis op. ed. His position is that core concern in the health sector is the critical condition of the public hospital system throughout Australia. He says that the three-hundred page reform ŌĆśblue printŌĆÖ from the National Health and Hospital Reform Commission:
has identified the major problem. The reality is that AustraliaŌĆÖs dangerously overcrowded public hospitals donŌĆÖt have enough beds to provide a safe and timely standard of care even for emergency patients. Unfortunately, the NHHRC has strongly supported a range of non-solutions. The primary care reforms it proposes will not help our dysfunctional State-run public hospitals cope with an inexorable rise in demand from an ageing population...As more and more people live to older ages, a tsunami of demand will break in public hospitals. Increasing numbers of ŌĆśvery oldŌĆÖ patients will inevitably require emergency and bed-based hospital care due to the age-related onset of chronic conditions...
His argument is that the wrong-headed premise of the Rudd GovernmentŌĆÖs reform agenda is that the Commonwealth must spend billions on a national network of comprehensive general practice ŌĆśSuper ClinicsŌĆÖ to take pressure off hospitals.
What Sammut and the CIS are opposing is the argument that there are some structural changes that offer openings for long-term changes in the way health is delivered ŌĆō away from the acute, hospital-centred model towards a system that puts more resources into prevention and care in the community.
Sammut's position is hospital centric. He argues in favour of rebuilding the hospital system with the Commonwealth taking full control of public hospital funding; introducing Medicare-issued, casemix-calculated hospital vouchers to pay for treatment in either public or private hospitals; state governments re-introducing local public hospital boards with full financial and administrative responsibility for their facilities; and closing down the area health services and use the money saved to fund vouchers and open and staff more hospital beds. It is a policy to reduce the health bureaucracy and put the savings into increasing beds in public hospitals.
Public hospitals need money to undertake reforms to become more efficient and safer for acute care. the case is compelling. It's now 15 years since the landmark Quality of Australian Health Care Study which found that 16.6 per cent of all hospital admissions were associated with an adverse event - half of which were considered "highly preventable". In March, Professor Jeff Richardson, of Monash University's Centre for Health Economics, updated those figures. He likens the number of such events today at approximately equivalent to one jumbo jet crashing every two weeks, each resulting in the deaths of 350 Australians. The cumulative unnecessary deaths since the publication of the QAHCS report would exceed the number of Australians killed in World War 1.
However, it is also the case that the health profile in our society has changed from episodic care to chronic health conditions (obesity, diabetes, mental illness, musculoskeletal conditions, ageing) and that the system is structured around hospitals providing relevant interventions for acute episodes. These chronic conditions are better managed within the primary care sector. Professor Hal Swerissen says:
The public hospital system should not be the first point of contact. It provides the backstop for the primary and community care system. If the first tier of the health system is not working well, then the hospital system will be put under stress.Not only will a stronger primary care system improve peopleŌĆÖs quality of life by preventing disease, disability and distress, it should reduce pressure on the public hospital system
The better the comprehensive care plan (integrating many different specialities), then the fewer acute episodes that should occur is the argument. Better access to primary healthcare will mean reductions in obesity and smoking and earlier and better treatment of chronic diseases, such as diabetes. Hence the need to shift away from the acute, hospital-centred model towards a system that puts more resources into prevention and care in the community.
Posted by Gary Sauer-Thompson at 9:44 AM | Comments (3) | TrackBack
July 22, 2009
health reform?
By all accounts the National Health and Hospitals Reform Commission, which has been Commission to deliver the 'biggest health shake-up in decades', has avoided recommending a federal takeover of public hospital funding in spite of Rudd Government previous threat to take over public hospital funding if the states failed to sign on to hospital improvements.
Instead the Commission recommends a shift to better --more effective---primary care to ease the strain on emergency departments of public hospitals. This is more a systematic reform rather than a bandaid:

It would seem that what has been recommended by the Commission is that outpatient services and community health centres now run by states would transfer to federal funding. This would aim to ensure a better coordination of services for patients between federally-funded general practitioners, the state-financed community centres and hospital out-patient services and the GP super clinics.
Better community services ( primary care) would reduce demands on the over-stretched hospital emergency departments. So keeping people out of hospital by preventing disease, improving access to GPs, and overhauling the aged care sector is at the heart of reforms.
Posted by Gary Sauer-Thompson at 1:59 PM | Comments (2) | TrackBack
July 10, 2009
Adelaide Festival Ideas 2009: health
One of the Sunday sessions at the Adelaide Festival Ideas is entitled Trick or Treatment? Alternative medicine on trial---It's a talk by Simon Singh, one of the authors of Trick or Treatment? Alternative Medicine on Trial. The session is in the form of a lecture not a debate.

The book is in the debunking tradition as the authors state in their introduction that "Our mission is to reveal the truth about the potions, lotions, pills, needles, pummeling and energizing that lie beyond the realms of conventional medicine."
The authors say their goal is to answer the question of whether alternative therapies provide any benefits ŌĆö or only a placebo effect TruthŌĆÖ is understood in the sense of the fundamental question: ŌĆśis alternative medicine effective for treating disease?ŌĆÖ This article by Singh in The Guardian with respect to chiropractic care is an example of the approach.
The book evaluates the scientific evidence for acupuncture, homeopathy, herbal medicine and chiropractic, and briefly covers 36 other treatments. It finds that the scientific evidence for these alternative treatments is generally weak, but finds that the acupuncture, chiropractic and herbal remedies have some evidence of limited efficacy for certain ailments. Homeopathy is concluded to be completely ineffective.
Their judgement is that this book delivers the ultimate verdict on alternative medicine. What they call conventional medicine is not under scrutiny because that falls under science, knowledge and truth whereas alternative medicine falls under opinion, ignorance and superstition.
According to a review in Frontier Psychiatristthis standard Enlightenment duality is defended in the following way:
Any treatment which cannot stand up to the rigours of scientific enquiry, by which Singh and Ernst mean a well conducted controlled clinical trial, has no place calling itself medicine and is simply hocus-pocus with good PR. At best such therapy is simply no better than placebo, at worse it is positively dangerous. But even if it is harmless, it is far from costless, as the annual global spend on alternative medicine is in the region of ┬Ż40 billion, money that could be spent on more fruitfully, should alternative therapies prove to be ineffective.
The position of the book is that anything that works and can be shown to do so in a properly conducted clinical trial is no longer actually alternative medicine, and anything which cannot pass these rigorous tests should be treated with great suspicion, since they are little more sugared placebo's.
Several quick points. The boundaries between orthodox and unconventional treatments are less precise than they suggest; complementary medicine has also become increasingly legitimised in the past decade; many people suffer from chronic illnesses that respond poorly to conventional treatments by orthodox medicine or from a constellation of symptoms that are not easily diagnosed or treated by mechanistic medicine; the randomized controlled trial is not the only way of gaining evidence in everyday clinical care, community health or building a knowledge base; no mention is made of the harm and deaths caused by orthodox medicine's interventions.
The appeal to well conducted controlled clinical trial is an appeal to the positivist, empiricist worldview that underpins the theory and practice of evidence-based medicine, and this overlooks the conflict within the long-standing ŌĆ£paradigm warŌĆØ in the philosophy of science between positivist, interpretivist, and critical approaches.
Posted by Gary Sauer-Thompson at 3:04 PM | TrackBack
June 21, 2009
US health care: reform
As Ezra Klein points out in American Prospect Obama's health-care reform is health-care-system-spending reform The purpose of health reform is to pay for health care -- not to improve the health of the population. If health insurance does not equal health, health insurance is important because, as Kein says:
for too many, a trip to the emergency room ends in bankruptcy, or a child's fall results in massive credit-card debt. And those who can't afford regular care often suffer terribly from chronic pain and preventable illness. Fixing the health-care system is imperative from both a moral and an economic perspective.
There are around 47 million individuals in the US currently uninsured and unable to afford care. Obama's public option if it materializes, will be just that ŌĆö an option Americans can choose, thereby giving Americans an alternative if private insurers fall down on the job.
 Kal
Kal
In the US Big Pharma and Insurance are planning to degut the public options in Obama's health care legislation that is before Congress--a public option that would compete with private insurers and use its bargaining power to negotiate better rates with drug companies. So it represents competition.
Posted by Gary Sauer-Thompson at 12:20 PM | Comments (5) | TrackBack
May 28, 2009
bio security
I guess the mainstream media doesn't understand the epidemology of how a global virus spreads since they have seen it as a bit of a beatup, scare mongering by the health authorities, or the angst of the worried well. Maybe the media thought that the word pandemic implies that the virus is lethal and capable of causing many deaths as well as meaning the global spread of the virus.
Pandemic is an epidemiological definition that has nothing to do with virulence. A pandemic of influenza occurs when a new viral strain emerges to which the population has little or no immunity.

The health authorities have lost the first stage of containment in preventing the virus from entering the country. Although currently it is only mild, the attack rate of the swine flu strain, which is a variant of the Influenza A H1N1 virus, is now affecting 23 countries is around 25-30%. There are now around 67 confirmed cases and around 4 million Australians are expected to suffer from it.
School closures, on the advice of the Health authorities are now a necessary part of the second stage of the containment strategy to limit the spread of the first mild wave (meaning hospitalization isn't necessary, not that it just produces a runny nose). At this stage we simply have a novel flu strain that has killed less than 1% of the people killed by the "normal" seasonal flu virus, even though it is likely to cause a pandemic as it spreads worldwide. But pandemic does not mean lots of deaths.
Some argue that the second wave of the virus will probably be more virulent. However, the effect with most viruses is that they usually become less aggressive with time not more. Secondly, the problem with the efforts to trace the contacts of everybody with the virus (the containment strategy) is that it quickly becomes unmanageable. So why the containment strategy instead of a 'sustain' strategy that treats the Influenza A H1N1 virus as a normal, seasonal flu?
So why all the politics of fear? Why the big beatup that scares people by the medical authorities when they know that the Influenza A H1N1 virus is mild? Their responses are out of proportion to what is a virus with only low levels of virulence. Treating this as seasonal influenza seems a more appropriate current response.
Posted by Gary Sauer-Thompson at 8:49 AM | TrackBack
May 23, 2009
economics of healthcare
In his article in the weekend edition of the Australian Financial Review on the econmics of health care Tom Dusevic sums up his key point thus:
To put it plainly Australians have to get real about ageing and health costs. Who pays for them?What level of service can we afford? Who gets treated? ....Centre for Policy Development director John Menadue says that we need governments to explain to the public that w e can't have all we want in health care. Resources are limited....He believes that unless we effectively and fairly manage demand, our spending on health will continue to realise poor value for money.
Menadue points out that rationing of services already happens and he cites the examples of hospital waiting lists, the neglect of indigenous health and mental health patients.
Dusevic works in terms of the wave of demand for healthcare from an ageing population and the unlikeliness of there being a dramatic jump in the allocation of funds to health. Hence the shortfall in funding and the solution --rationing.
Posted by Gary Sauer-Thompson at 11:55 AM | Comments (11) | TrackBack
May 1, 2009
fear
Though I don't discount the possibility of a pandemic and support the precautionary public heath measures to prevent the spread of the Influenza A H1N1 (swine flu) virus, there is still an element of politics in this that plays into the politics of fear.
The politics is the constant repetition that The BIG ONE (apocalypse) is coming and this could be it. Then there is the standard reference back to the 1918 influenza pandemic, despite the differences: the existence of antiviral drugs, antibiotics or vaccine. The element of politics is scaremongering. This is it. These things happen in natural cycles.
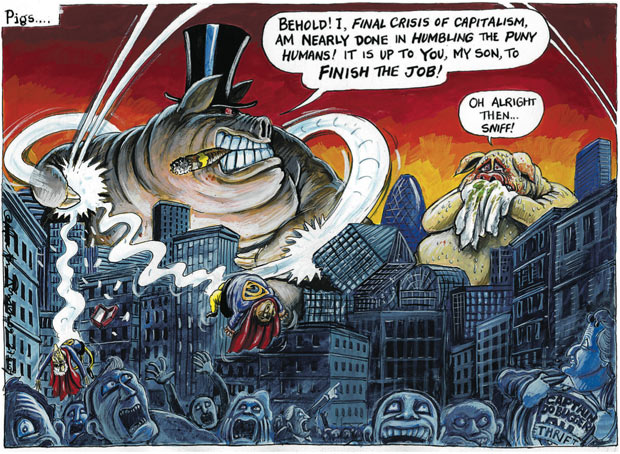 Martin Rowson
Martin Rowson
The media have certainly played it up even though the normal annual influenza kills far more people than the swine flu.In a typical year, 36,000 people die in the US from flu-related complications. Some 10,000 people die of influenza every year in Britain during the normal winter flu season.Every year approximately 10,000 Mexicans die from the effects of seasonal flu. The vast majority of the reported cases of Influenza A H1N1 have made a quick and full recovery after a mild and short illness.
Why the big fear then, when there there is no reason, as yet, to believe that we are on the brink of a similar disaster as 1918?
Sure, the target population that is dying from this is different from the normal flu, in that it is not the very young and old. But a pandemic? The number of cases world wide is low (275) as are the number of deaths (160) and 159 of those were in Mexico.
Someone says that up to 40% of the world could be infected. Others say that 120 million could die. How in the hell do they know? The epidemiological data is just not there. We do not know. Nor are we sure what the virus is. Is it actually the new emergence of a triple human-swine-bird flu virus? Or a variant on a hybrid virus we have seen before? Yet we have fantastical scenarios flowing through the airwaves and newspapers---an unconscious collective dread surfacing in the media.
Update
The standard reference to natural cycles in reference to influenza pandemics happening in 1889, 1918, 1957 and 1968 is also misleading. What is right is that through human history, viruses have mutated, and sometimes they have taken nasty forms that have swept through the human population. This is an inescapable natural reality we just have to live with, like earthquakes and tsunamis. However, things have shifted with industrial factory farms, as these become the incubator for viruses and their mutation. Thus:
In most swine farms today, 6,000 pigs are crammed snout-to-snout in tiny cages where they can barely move, and are fed for life on an artificial pulp, while living on top of cess-pools of their own stale faeces ... the virus now has a pool of thousands, constantly infecting and reinfecting each other. The virus can combine and recombine again and again. The ammonium from the waste they live above burns the pigs' respiratory tracts, making it easier yet for viruses to enter them. Better still, the pigs' immune systems are in free-fall. They are stressed, depressed, and permanently in panic, making them far easier to infect. There is no fresh air or sunlight to bolster their natural powers of resistance. They live in air thick with viral loads, and they are exposed every time they breathe in.
Instead of a virus only having one spin of the roulette wheel, it has thousands and thousands of spins, for no extra cost. It drives the evolution of new diseases. With the massive concentrations of farm animals within whom to mutate, the new swine flu viruses in North America appear to be on an evolutionary fast track, jumping and reassorting between species.
Update: 2
For those interested in the more scientific medical aspect of the flu virus could start by looking at the virology blog run by Vincent Racaniello, Professor of Microbiology at Columbia University Medical Center. He talks in terms of a novel strain of H1N1 swine influenza virus and adds:
The influenza season is nearly over in the northern hemisphere - it usually does not continue beyond May. Increasing temperature and humidity are likely to curtail transmission of the virus very rapidly. The same virus could return in the fall, but by then a vaccine could be produced and distributed.The southern hemisphere is another story - the influenza season there is just starting. It is certainly possible that this swine virus might cause extensive epidemics.
The phrase"'novel strain" is crucial since pandemic influenza has always been a consequence of viruses of a new subtype whereas the swine virus is of the same subtype as the currently circulating human H1N1 strain.
Posted by Gary Sauer-Thompson at 9:30 AM | Comments (9) | TrackBack
March 18, 2009
The Senate acts
It's good to see the Senate doing its job properly --using its powers responsibly to improve government legislation and to push the government further down the reform pathway to ensure the public interest or a public good. The crossbench is crucial to a long list of bills the Rudd Government wants passed, and it is far from being recalcitrant or dithering or obstructionist.
A good example is the Allcopops legislation, where the Greens and independent senator Nick Xenophon have used their power to persuade Health Minister Nicola Roxon to set aside an additional $50 million from the $1.6 billion raised for measures to tackle alcohol abuse. Why would the Rudd government resist that proposal,when its concern is to stop teens from binge drinking.?
The agreement includes the creation of a $25 million health sponsorship fund to provide support for sporting and cultural activities as an alternative to alcohol sponsorship, mandatory warnings on alcohol advertising, community-level initiatives to tackle binge drinking and enhanced telephone counselling services and alcohol referrals. Alcohol is connected to a health and can cause health problems.
The interpretation of this legislation by Bernard Keane, Crikey's Canberra correspondent, is that:
its lasting political significance will be no more than that of another stunt, Fuelwatch, which fell by the wayside last year after inquiries, theatrics and Parliamentary ranting, and was promptly forgotten.
Keane does appear to behold the view that the Rudd Government has its agenda ensnared in Senate obstructionism and that the House of Represenatives rules. That how he interprets the Rudd Government needing to negotiate its key legislation through the Senate,
However, he misses the point of the allcopops issue. These may be small reform steps in taxing alcoholic lollywater, but they represent a break with the laissez-faire approach to alcohol advertising that paid no attention to the negative effects of alcohol. Keane misses the political symbolism of this, and the explicit rejection of the libertarian position that holds the "nanny state", or wowsers, or do-gooders are dictating how much people should drink or setting upper limits to drinking for everyone.
The Senate is acting because the full cost of alcoholic lollywater is not borne by the producer (Big Alcohol). This is the negative externality problem in economic language, and it challenges the view that the allcops tax is just the Rudd Government utilizing coercion for a tax grab (plunder) at the expense of individual liberty. What we have with allcopop is a political solution to market failure.
Family First senator Steve Fielding wants to push this issue further: to address alcohol advertising during sports programs on television.He wants the Government to close a loophole that permits television advertising of alcohol during family viewing time in sporting broadcasts. For once, Fielding has adopted a reasonable position. The implication is that the laws covering the banning and other restrictions on grog marketing and sponsorship do need to be tightened progressively.
Economic libertarians (the utilitarian variety) would argue against these government policies on the grounds that they exceed the bounds of the minimal state. They would oppose these laws on the grounds that they prohibit certain types of exchanges as well burdening exchanges by imposing high transaction costs. Some would argue that today's market failures will provide the opportunities for tomorrow's entrepreneurs to profit by new innovation. What they need to argue is that such policies to prevent market failure will not produce greater utility than a policy of laissez-faire.
Posted by Gary Sauer-Thompson at 8:01 AM | Comments (10) | TrackBack
February 19, 2009
A Healthier Future for all Australians: key proposals
The National Heath and Hospitals Reform Commission's interim report---A Healthier Future for all Australians is the first major cut at reforming the heath system; a reform process that has been consistently opposed by the AMA and the private insurance industry. Reforming and refocusing health-care systems is difficult, and new ideas provoke stakeholders' prejudices and vested interests.
The key proposals of the interim report are:
- Commonwealth takeover of primary care
- Universal dental scheme, called Denticare Australia, funded by an increase in the Medicare levy
- Accommodation bonds be permitted for high care residents in aged care facilities
- Nurse practitioners and other health professionals in remote and rural areas to be able to provide services covered by Medicare and prescriptions covered by the Pharmaceutical Benefits Scheme
- Creation of a patient-controlled e-health record, which could be accessed, with the patient's agreement, by multiple health professionals
- Delivery of wellness and health promotion programs by employers and private health insurers
- A youth-friendly community-based service to provide information on sexual health and mental disorders to be rolled out nationally
- A share of commonwealth hospital funding to the states to be tied to meeting or improving progress performance targets, payable as a bonus
-Three options were suggested relating to the structure of the health system. The most radical option is a commonwealth takeover of the system, with compulsory social insurance
This is a first cut since it does not integrate physical health and mentally health and avoids the opportunity costs implicit in the $4 billion spent annually on private health insurance rebates. The centre piece of the National Heath and Hospitals Reform Commission's reform is oral health-----bringing it into Medicare in the face of opposition from the dentists. Denticare is universal dental insurance that is funded by increasing the Medicare levy by 0.75 per cent.
The Australian Dental Association argues that the Government should target the 35 per cent of the community who could not access or afford proper dental care and said it would be fiscally irresponsible to introduce a universal scheme for dentistry.The Association for the Promotion of Oral Health argued that the Denticare scheme would create a two-tiered system, whereby federal funding would be simply given to the private system.
Update
Alan Fels in The Age makes some good points about workforce issues. He says:
For too long, the health industry has relied on 19th and 20th century financing models and rigid professional roles to deliver 21st century care. The Prime Minister went to the last election promising real reform. But the real issues go well beyond resolution of federal and state responsibilities.The lesson from the 1980s and 1990s in other non-responsive industries was that real increases in productivity and improvements in quality were hard to achieve without genuine workforce reform....Sadly, our Medicare system pays top dollar for single practitioners to work on their own and see the same people each time they come back for care. The system actually penalises those who spend real time with those in trouble and those who work with other health professionals.
Australia is stuck in a mode of service delivery based on historic professional roles in which health professionals have jealously guarded their roles for a long time. As with all industries, there comes a time for a fundamental rethink of the way human resources are deployed, roles, responsibilities and reimbursement.
Posted by Gary Sauer-Thompson at 5:53 AM | Comments (1) | TrackBack
February 16, 2009
health reform
The National Health and Hospitals Reform Commission will release a 400-page interim report today containing proposals for a shake-up in health which will be refined in its final report to the Government in the middle of the year.
Media reports say that the Reform Commission is calling for a radical revamp of Australia's public health services and a bigger federal role in community-based health care, dental services and aged care. It proposes the establishment of "comprehensive primary health care centres" - a larger-scale version of the Government's plans for 31 GP super clinics - to provide one-stop-shops for care by GPs, nurses, diagnostic services, family and child health and other professionals such as physiotherapists, psychologists and podiatrists.
The emphasis is on more intergrated and comprehensive care within a coherent national policy with identified goals and strategies supported by adequate funding. No doubt this will be opposed by the AMA, who have opposed the first steps in this direction with the formation of the GP Plus centres.
Posted by Gary Sauer-Thompson at 6:05 AM | Comments (2) | TrackBack
January 30, 2009
NSW health: broke
The deeply divided, conflict ridden NSW Government seems to go from bad to worse. Its health system--eight area health services and the Children's Hospital at Westmead--- is broke and unable to pay bills. There was $117.5 million in overdue invoices across the system at the end of this month. No worries the health Minister has got it all covered.

Despite the NSW Government spin the "service is so strapped for cash that it is not even paying doctors. Presumably this is the result of a deliberate neo-liberal policy of squeezing the health system.
Posted by Gary Sauer-Thompson at 5:47 AM | TrackBack
January 5, 2009
drugs, doctors, disease
In Drug Companies & Doctors: A Story of Corruption in the New York Review of Books Marcia Angell, a former editor of the New England Journal of Medicine, highlights a disturbing trend in modern medicine. She says:
No one knows the total amount provided by drug companies to physicians, but I estimate from the annual reports of the top nine US drug companies that it comes to tens of billions of dollars a year. By such means, the pharmaceutical industry has gained enormous control over how doctors evaluate and use its own products. Its extensive ties to physicians, particularly senior faculty at prestigious medical schools, affect the results of research, the way medicine is practiced, and even the definition of what constitutes a disease.
The conflicts of interest in medicine are deep and pervasive given the dependence of the medical profession on the pharmaceutical industry.
The redefining of disease refers to the way that drug companies have perfected a new and highly effective method to expand their markets. Instead of promoting drugs to treat diseases, they have begun to promote diseases to fit their blockbuster drugs. The strategy is to convince as many people as possible (along with their doctors, of course) that they have medical conditions that require long-term drug treatment.
Some of the biggest blockbusters are psychoactive drugs. The theory that psychiatric conditions stem from a biochemical imbalance is used as a justification for their widespread use, even though the theory has yet to be proved. Children are particularly vulnerable targets. What parents dare say "No" when a physician says their difficult child is sick and recommends drug treatment? The consequences is that:
physicians learn to practice a very drug-intensive style of medicine. Even when changes in lifestyle would be more effective, doctors and their patients often believe that for every ailment and discontent there is a drug. Physicians are also led to believe that the newest, most expensive brand-name drugs are superior to older drugs or generics, even though there is seldom any evidence to that effect because sponsors do not usually compare their drugs with older drugs at equivalent doses. In addition, physicians, swayed by prestigious medical school faculty, learn to prescribe drugs for off-label uses without good evidence of effectiveness.
Angell says that breaking the dependence of the medical profession on the pharmaceutical industry will take a sharp break from an extremely lucrative pattern of behavior. But if the medical profession does not put an end to this corruption voluntarily, it will lose the confidence of the public, and the government will step in and impose regulation.
Posted by Gary Sauer-Thompson at 7:28 AM | Comments (4) | TrackBack
November 28, 2008
NSW Health: Garling Report
On the eve of CoAG there is the promise for extra Commonwealth funding for health care in the form of a new five-year health funding agreement between the Commonwealth and the states designed to end the blame game.
The states' demands are for extra funding. They are seeking a more realistic indexation arrangement and a restitution in the key area of public hospital funding of the 50-50 funding split that was eroded under John Howard and Peter Costello. The federal government funds about 42 per cent of public hospital services. The states are also seeking a one-off catch-up payment to reflect poor deals in the past on public hospital share and indexation.
More than extra funding is needed. The recently released Garling Report into hospitals in NSW indicates that the states need to reform the way health is delivered. Commissioner Peter Garling, SC, said that though the NSW had a public hospital system of high standard, that system was on the brink of collapse:
Given the demographic changes and the rising costs, it is the case that we have entered into a period of crisis for a public hospital system which has always been free and accessible to all. If public hospitals are to survive as providers of free care for all, there will have to be some radical changes in the way they do business. We are on the brink of seeing whether the public system can survive and flourish or whether it will become a relic of better times. To start with, a new culture needs to take root which sees the patientŌĆÖs needs as the paramount central concern of the system and not the convenience of the clinicians and administrators.
So it is not just a case of more money from the Commonwealth to maintain real rates of growth in funding in the face of an ageing population and technological change. Radical changes are needed. What are these?
For Michael Costa this involves the federal Government having responsibility for all aspects of national health care, including funding and administration of the public hospital system. Plus hospital-level competition on quality and cost effectiveness of service provision should be introduced with resources flowing to the best hospitals.
Garling takes a different tack. He says radical reform includes new models of care at the clinical unit level at the state level:
The doctors, nurses and allied health professionals will need to replace the old system where different specialists would see the patient but no one person would necessarily take complete charge of the patientŌĆÖs care. A new model of teamwork will be required to replace the old individual and independent ŌĆ£silosŌĆØ of professional care. Furthermore, the rigid demarcation between what a doctorŌĆÖs job is, and what a nurseŌĆÖs job is, needs to be consigned to history. Once the concept of teamwork is accepted as the norm in treating a patient, it is easier to see why a qualified nurse practitioner should be able to do many jobs once reserved for doctors.
This means the changing of a professional culture and this can only occur if the why and wherefore of reform is taught in the undergraduate and early clinical training years. This means the creation of a modern, well trained, flexible hospital workforce.
This reform needs to be backed up investment in informations technology so that the information collected is to be directed to how well the patient has been treated, not to process-driven, often politically-driven, data which may make administrators more comfortable, but not the patients.
In contrast to Costa's top down reform model Garling says:
that redesign of clinical practices must be a bottom-up reform driven by clinicians; that information about the safety and quality of treatment at the unit level is the greatest guarantee of a quick change-over to evidence based best practice models of care; that the only way to avoid a slide of the present clinical standards into mediocrity or worse is by strengthening the training of new clinicians in better, safer treatments based on a patient centred team approach; that the safety and quality of public hospital care should be the highest priority of the public hospital system, and that its employees need to implement this at the individual patient level.
Garling adds that know that, as a rule, a person with an illness is often better off being treated outside rather than inside a hospital. Of course this does not apply to someone who suffered a serious accident or has taken the wrong medication or is suddenly struck with chest pains. But the bulk of chronic conditions are
better dealt with in the home or in the community than in an acute care bed.
Posted by Gary Sauer-Thompson at 4:58 AM | Comments (2) | TrackBack
November 9, 2008
Sunday cartoon: indigenous health
One of the pillars of the initial phase of the Northern Territory Emergency Response from a health point of view was the health checks carried out on up to 17 000 children aged 15 years and under in 73 target communities. The health checks were designed to bridge the seventeen-year mortality gap for all Indigenous people. By 19 October 2007, medical teams had already completed checks on more than 3200 children.
 Golding
Golding
What happens after the health checks? Those who are sick need treatment. How is that to happen? Fly in specialists?
William J H Glasson, a member of the emergency response taskforce, wrote in the Medical Journal of Australia:
The findings of these checks are sobering, and underline the need for the intervention. We already knew that the children in many of these communities had very high rates of chronic diseases, but have found that the situation is even worse than the official picture. The Indigenous population has a burden of disease up to six times higher than in the non-Indigenous population.
Probably 80% of the Indigenous children have middle-ear diseases. Intestinal parasites and skin infections are rife. An absence of water for washing ŌĆö taps donŌĆÖt run, toilets donŌĆÖt flush, there is no soap ŌĆö has led to skin hygiene so poor that pathogens thrive. This in turn contributes to the devastating levels of renal disease and heart disease, the latter particularly associated with rheumatic fever. Type 2 diabetes is also increasingly common in children.
The call has now gone out for health professionals, doctors, specialists and nurses to help out with the follow-up, but this type of approach to the delivery of needed health services is an emergency response and is not sustainable. Something more is needed.
Posted by Gary Sauer-Thompson at 11:08 AM | Comments (7) | TrackBack
October 18, 2008
NSW by elections
It would appear that the dysfunctional Rees Government in NSW is going to suffer some body blows from voters wielding baseball bats in the byelections in the safe seats of Cabramatta, Lakemba and Ryde. Huge swings are expected.
And why not.This is an incompetent corrupt state government that does not deserve to be in power. An example. As the Sydney Morning Herald says:
Supplies are so scarce at Dubbo Base Hospital that it is borrowing bandages from the local vet...Just three weeks ago, a doctor had to use $770 of his own money to buy reagent for urgent blood tests because the hospital had run out of credit with the supplier, while endoscopies have had to be rescheduled for lack of sterilisation fluid. There are also routine shortages of such basics as surgical gloves and garbage bags. This would not be acceptable in a clinic in a remote corner of a Third World country, let alone at a 134-bed teaching hospital in a major regional centre of NSW.
The reason for the lack of supplies is that NSW Health does not pay the bills. This is not an isolated case. The Herald says that tens of millions of dollars are currently outstanding to suppliers from half of the state's area health services: Greater Western (covering Dubbo), Northern Sydney/Central Coast, South Eastern Sydney/Illawarra and Greater Southern. Patient safety is compromised by a refusal to pay bills by the NSW Health Department since many suppliers now refuse to grant credit to NSW hospitals.
NSW Health refuses to reveal how much it owes. It's crisis management response is to gag its area health services. Presumably NSW Health has no money or it is incompetent. Either way the NSW Government deserves to be thrown from office.
Posted by Gary Sauer-Thompson at 9:06 AM | Comments (15) | TrackBack
September 26, 2008
adverse events in Australia's public hospitals
Finally it is coming out-----adverse events in the health system that are preventable. The Australasian College for Emergency Medicine has said that research shows that overcrowding and delays in moving patients from emergency departments to a hospital bed caused 1500 extra deaths nationally.The claim is that more people die from hospital overcrowding and admission logjams than in road accidents. This is not the kind of news that state politicians want to be made public.
The claims have escalated into a furious row between senior doctors and the SA state government. In SA a senior emergency specialist, Tony Eliseo, claimed the crisis was costing 150 lives a year in SA alone, rivalling the road toll. John Hill, the Minister of Health, is outraged and rejects any comparison between road toll and hospital-related deaths. Pure theory put about by academics is his rather implausible response.
If it is 150 deaths in SA, then how many die in WA from access blocking and overcrowding?
ŌĆ£Access blockŌĆØ is defined as the situation where patients are unable to gain access to appropriate hospital beds within a reasonable amount of time, no greater than 8 hours. ŌĆ£OvercrowdingŌĆØ refers to the situation where Emergency Department (ED) function is impeded by the number of patients waiting to be seen, undergoing assessment and treatment, or waiting for departure, exceeding the physical or staffing capacity of the department.
The literature review undertaken by the Australasian College for Emergency Medicine states that:
The most vulnerable individuals affected by access block and ED [emergency department] overcrowding are those who due to their medical conditions require unplanned admissions to hospital. The most common groups include: the elderly, particularly those with chronic and complex conditions; people
arriving by ambulance; people visiting EDs after hours or on week-ends; children and parents of
young children; mental health patients; drug and alcohol patients; nursing home patients;
people without social support; patients with medical conditions exacerbated by seasonal
changes; people with painful conditions; the undiagnosed critically ill; seriously-ill patients who
leave without being seen by a doctor; and patients who are inappropriately discharged from
hospital in order to increase bed availability.
Access blocking and overcrowding result from there being not enough available beds to meet demand.
ED overcrowding. This is associated with significant mortality and human suffering.
Posted by Gary Sauer-Thompson at 4:41 PM | TrackBack
September 25, 2008
Senate blocks change to Medicare threshold levy
I understand that the budget changes to the Medicare levy surcharge threshold were defeated by a single vote from Victorian Family First senator Steve Fielding.This was in spite of last-minute changes to the proposed legislation by Health Minister Nicola Roxon on Tuesday, which altered the new threshold for singles from $100,000 to $75,000.
So Family First sides with Coalition to block this compromise, which was based on indexing the Coalition's 1997 thresholds. It is the equivalent to a tax cut, and the Liberals are in the position of opposing tax cuts to prop up the private health insurance industry.Had the Bill passed, it would have delivered up to $1200 of tax relief to 330,000 people.
Senator Fielding defends his move by saying the Government had done nothing for lower-income earners who could be affected by higher health insurance premiums:
When you change it, you've got to be really careful that you look after those who will be worse off..hese are people vulnerable Australians, low-income earners and pensioners that are now going to have the rug pulled out from under their feet.
Yet health insurance premiums would be 2.5% p.a. (roughly $20) whilst around 70% of lower income earners do not have private health insurance. So Fielding is defending corporate welfare in the form of rent seeking from tax payers.
Health Minister Nicola Roxon will stare down the Senate, introducing redrawn Medicare legislation that will give effect to her compromise plan to slash a proposed increase in the Medicare levy income threshold from $100,000 to $75,000.
Posted by Gary Sauer-Thompson at 8:52 AM | Comments (4) | TrackBack
September 22, 2008
health reform: looking good
As is becoming increasingly clear the Rudd Government's health reform aims to reduce health inequality and increase access to good health care. Inequality means poor health and poor health means inequality. The commitment to reform clashes with the interests of doctors as it seeks to remake the role of general practitioners and how health funding is delivered to the states.
What the reforms seek to do around primary care is for nurses, psychologists, physiotherapists and dieticians to take on more work traditionally performed by doctors. This directly attacks the way that the health system has been organized around doctors and the way that health care is funded by Medicare.
In a recent speech entitled 'The Light on the Hill: History Repeating', given as an address to the Annual Ben Chifley Memorial Light of the Hill Dinner in Bathurst, Nicola Roxon, the Minister of Health and Ageing, argues that prevention a key weapon in the arsenal of health. Investing just in hospitals can play only a very limited role in addressing disadvantage. It can do a great deal of good, but the chance at early intervention, and a better life, has been lost. It is the notorious ambulance at the bottom of the cliff ŌĆō not the fence at the top that stops the fall in the first place.
Roxon goes on to say that our health system, including funding for health services, is organised almost entirely around doctors, despite the fact that many services are now safely and ably provided by other health professionals ŌĆō nurses, psychologists, physiotherapists, dieticians and others:
Doctors must and will remain central to our health system. But to date, professional resistance and government funding have prevented the development of a health sector in which services are delivered not only by doctors, but by other health professionals who are safe, potentially cheaper and, most importantly, available....Doctors will need to be prepared to let go of some work that others can safely do. To ensure this transition, there needs to be an incentive for doctors to eschew less complex work, and focus on the work that does require their high-level skills and expertise. Or if doctors do not want to let go of it, to accept being paid less for devoting their highly skilled and heavily trained selves to less complex tasks then they might.
So the reform thrust is to addresse the historical bias towards medical intervention and acute care by shifting the focus of the health system to prevention and to explore the ways in which nurses and allied health professionals can take on some of the work of GP's.
Posted by Gary Sauer-Thompson at 9:03 AM | Comments (5) | TrackBack
September 18, 2008
Senate debates Medicare Ley Surcharge
The ALP's Medicare Ley Surcharge threshold bill is in trouble in the Senate The Rudd Government wants to raise the income thresholds determining liability for the 1 per cent surcharge from $50,000 to $100,000 for singles and from $100, 000 to $150,000 for couples. Both Xenophon and Fielding are saying 'hang on a mo' folks, not so fast.
Nick Xenophon said he would block the bill on the grounds that the increase would likely lead to an exodus of members from the private health funds, increase pressure on public hospitals, and lead to higher premiums for those who retained private health insurance. His position is that he wants the government to index the income threshold of its original base, which means that the surcharge kicks in at $67,000 for singles and $134,000 for couples. Grounds for negotiation one would think.
Steve Fielding had similar concerns about an exodus from private cover and rising premiums for those who remained. He said that his support for the bill was contingent on the government agreeing to raise the private insurance rebate by 5% to help lower income income earners who might face higher premiums. He made no mention of what constitutes low income.
Compromise is clearly needed. The Rudd Government is showing little inclination to negotiate as it spends lots of its energy attacking the Liberals for not supporting its measures in the Senate. Why bother? The Liberals have clearly said they strongly stand behind private health insurance and oppose its undermining. That means negotiating with Xenophon, Fielding and the Greens on the narrow issues of threshold.
The ALP's cost saving rhetoric is a furphy. The real issue is the ALP shifting the emphasis from private to public health and spending lots more money on public health care.Their best line of attack is to point out the hypocrisy of the free market Liberals in providing public subsidy for private health insurance industry when they oppose it for the manufacturing industry to prevent it from going offshore.
The private health funds need to lift their game in terms of product. After all, their commitment to the free market and the disciplining effects competition means they stand or fall on meeting the demand for private health care with good product. What they offer can be improved. Good product would help prevent the exodus from private health insurance.
Posted by Gary Sauer-Thompson at 6:50 AM | Comments (2) | TrackBack
September 13, 2008
The happy industry
According to The Guardian Big Pharma is worth ┬Ż600bn, it pushes products to doctors, who are supposedly trained to spot drug company nonsense. The food supplement industry (vitamin pills and herbal supplements) is worth ┬Ż30bn, and is marketed with sciencey-sounding rhetoric, through the media, and no regulator rarely evaluate their claims.
The supplement industry is marketed as a cottage industry, is linked to the "nutritional therapists" community who often make claims on poor evidence. The lack of regulation is compounded by the lack of national registration and accreditation.
If there is a need to ensure the regulation of the food supplement industry, then the medical thinking behind medication, quick fixes and doping the populace for mental illness also needs to change. The drug companies are marketing fear in order to re-define human illness. In alliance with company-friendly doctors and sponsored patient groups, the all-powerful pharmaceutical industry is helping to widen the very definitions of disease, in order to expand markets for its drugs. the over-medicalization of mental disorders and the overuse of medications is often the result of the way that financial incentives and managed care have contributed to the notion of a "quick fix" by taking a pill.
It is true that the effectiveness of antidepressant, mood-stabilizing, and antipsychotic medications has helped sensitize the public to the reality of mental illness and taught them that treatment works. In this way, Big Pharma has helped reduce stigma associated with psychiatric treatment and with psychiatrists. However, it does look as if psychiatry has been almost completely bought out by the drug companies and they often come across as prescription writers -- ciphers in the guise of being "helpers".
This turn to drugs has reduced the emphasis on psychotherapy and psychosocial treatments. The overmedication and overmedicalization as a result of the commercialization of health care by Big Pharma means that there is a serious decline in the interest in and practice of so-called talk therapy, a process that attempts to understand the in-depth source of people's emotional reactions, unconscious motivations and internal conflicts. There is also an increased reliance on antidepressants and short-term cures that are not only impersonal but inadequate.
Although medication and other shortcuts have certain value in conjunction with therapy and are sometimes essential, they generally represent only symptomatic cures and fail to address the deeper emotions and conflicts that produced them. These internal conflicts are likely to persist and continue to harm people's relationships, children, work habits and overall quality of life.
The turn to drugs is part and parcel of the theory that the great majority of common psychiatric conditions (such as depression or psychosis) are caused by underlying disturbances in brain function. The medical model of mental illness postulates brain pathology as the basis for mental illness.
Posted by Gary Sauer-Thompson at 8:55 PM | Comments (6) | TrackBack
September 10, 2008
Medicare Levy surcharge
The Senate's Economics Committee has handed down its report into the Rudd Government's raising of the Medicare Levy Surcharge (MLS) Threshold for people without private health insurance.
The bill proposed to increase the Medicare levy surcharge threshold for individuals from $50 000 to $100 000 and for couples from $100 000 to $150 000. The increased thresholds will apply from the 2008ŌĆō09 year of income and later years of income. The overriding consideration was the danger of forcing an ever larger number of low-income people to pay the MLS or to buy low value fund policies for which they have little use, due to the threshold being unindexed since 1997.
The points of contention are structured around the possible impact of the bill on membership of private health funds, subsequent premium increases and the consequent cost to public hospitals as a result of the proposed increase in the Medicare Levy Surcharge (MLS) thresholds.
The core argument of the private health insurance industry is that the bill upsets the delicate balance in the Australian health system between public and private health provision. The crux of this argument is the claim that without a strong private health insurance industry, the provision of private health services will falter and lead to a flood of demand into the public system which it would be unable to meet.
If there is to be a public subsidy to maintain the "delicate balance" then the funding should have been provided to the private hospitals themselves, rather than the funds. We are in effect subsidising the insurers-- the insurersŌĆÖ administrative costs and surpluses when all but one of them are now large profit-making businesses.
In his op-ed in the AFR Terry Barnes, a former ministerial staffer and now a policy consultant, argues that Rudd's health policy is a basket case. He says:
Senior bureaucrats see inexperienced new governments coming. Treasury and Finance hate the non-means-tested PHI [private health insurance]. It is anathema for them--an open-ended appropriation, driven by demand. They consider its success a triumph of populism over prudence, even though it helped save the private health sector from collapse. But this year a new government with an ambivalent view of private health was preparing its first budget and looking desperately for savings. In opposition it had railed against the perceived injustice of the unindexed surcharge thresholds.Once again savings on the rebate were offered. This time to Wayne Swan not Peter Costello. This time they were accepted with alacrity.
Barnes adds that it was a measure that could be dressed up as a fiscally responsible tax break on the one hand, and keeping faith with Labor's anti-PHI constituency on the other, was a an added political bonus. Labor's health policy is a basket case because it faces defeat in the Senate and it is not sensible.
So there you have the Coalition's health policy--prop up the private insurance industry at all costs.
Posted by Gary Sauer-Thompson at 10:31 AM | Comments (4) | TrackBack
August 8, 2008
corporate medicine
One of the changes in primary care is the rise of corporate medicine over the last 10 years. The corporates hoped that by setting up medical centres with GPs, pathology and radiology facilities and sometimes allied health-care workers, these would make money from a process of internal cross-referrals. GPs would refer their patients for pathology tests and X-rays to the in-house facilities, and some referrals could also flow the other way.
 For these medical centres to work, the corporates had to get GPs into them and money was paid, sometimes quite big sums, to lure the GPs in. For a lot of older doctors and some young ones too, this was a chance for them to pay off their mortgage and have something to put into their superannuation.
For these medical centres to work, the corporates had to get GPs into them and money was paid, sometimes quite big sums, to lure the GPs in. For a lot of older doctors and some young ones too, this was a chance for them to pay off their mortgage and have something to put into their superannuation.
The new model medical centres are often open six or seven days a week and are usually open for extended hours every day. They all bulk-bill. A lot of them don't take appointments for their doctors. Patients therefore have to queue up and wait, and if a patient chooses to see a particular doctor rather than the first doctor available, then that obviously means an even longer wait.
The emphasis is towards encouraging loyalty to the medical centre rather than loyalty to the one doctor. Tuck Meng Soo, a Canberra GP, describes how the corporates work in The Canberra Times:
If a patient comes in for a check-up for her diabetes or to discuss the complications of her latest antidepressant medication and the consultation takes 20 minutes, the GP still gets $32.80 from Medicare. So, for a corporate to maximise income for itself and the GPs working there, they need to encourage patients with chronic and complex problems to seek health care for their conditions elsewhere and to encourage as many six-minute consultations as possible. This is precisely what the structure of the corporate medical centres does.
As more GPs are seduced into working for corporates, the non-corporatised GPs are left with an increasing caseload of patients with chronic and complex problems with the ''easy'' coughs and colds that used to leaven their day taken away. At some point, the burden of work and responsibility gets too much to bear and many non-corporatised GPs just give in and leave medicine or join the corporates.
Posted by Gary Sauer-Thompson at 3:51 PM | Comments (3) | TrackBack
July 8, 2008
alternative health care
In the 2006-2007 financial year, Medicare Australia paid out more than $23 million in rebates for patients who received acupuncture, chiropractic therapy and osteopathy. While only a small number of people qualify for the rebates ŌĆō those with chronic conditions and with complex care needs ŌĆō the cost to the public purse could rise dramatically if complimentary and alternative Medicine (CAM) becomes part of mainstream medicine as forecast by some within the medical fraternity.
More than $4.1 billion is spent nationally on CAM, with up to two-thirds of the Australian adult population using at least one product and one in four using complementary medicine services.The most frequent users are the better educated, higher-income earners, middle-aged women and people suffering with chronic and painful conditions that orthodox medicine manages poorly
Rose Shapiro's Suckers: How Alternative Medicine Makes Fools of Us All, argues that alternative medicine can jeopardise the health of those it claims to treat, that it leaches resources from treatments of proven efficacy, and remains largely unaccountable and unregulated. It is an industry (Included in alternative medicine are acupuncture, chiropractic therapy, homeopathy and herbal medicine) preying on human vulnerability, whose success makes fools of us all. The title casts consumers as gullible and practitioners as vampiric and we consumers spend billions each year on what amounts to little more than snake oil because our critical faculties are dulled by the pleasures of having someone listen to us.
Two things are notably lacking in dismissal texts such as these (another is Trick or Treatment: Alternative Medicine on Trial by Simon Singh and Edzard Ernst) that work the Enlightenment's science v religion duality. The first is an acknowledgement of the problems of funding adequate trials so that this health care, like medicine, becomes evidence-based, and, secondly, a discussion of the equivalent risks and inadequacies of conventional medicine. Though extensively tested, pharmaceutical drugs are scarcely devoid of side effects, and patient dissatisfaction with their treatment options is one of the many reasons why alternatives have become so popular.
The prevailing mechanistic model is not good at treating patients suffering from chronic illnesses that respond poorly to conventional treatments or from a constellation of symptoms that are not easily diagnosed or treated. These include 'headaches, heartaches, backaches, aching feet, fatigue, anxiety and those vague burning pains in your legs at night - and mechanistic medicine says that t there is no reliable cure for any of them'. So we ignorant consumers are obliged to put up with our headaches, backpain, heartaches and depression and stay unwell.
It is often argued that faith based medicine relies on obsolete or metaphysical concepts of human biology and physiology that have to be described as absurd. Obsolete here means not mechanistic, which means vitalism or organic. Secondly, it is argued that proponents of such concepts as vitalism or process philosophy will not subject their interventions to scientific scrutiny, suggesting that the mere attempt of critical evaluation is sufficient to chase the healing process away. So CAM is dumped in the dustbin market irrational.
Things are shifting. At an international CAM congress staged in Sydney earlier this year, the Federal Government announced more than $7 million in grants for the creation of new centres and research projects across the country. In Queensland, more than $660,000 was awarded to establishing a new clinic at the University of Queensland in a bid to integrate CAM with conventional medicine. Maybe research will be conducted to see develop evidence about which forms of alternative health care is effective.
Posted by Gary Sauer-Thompson at 8:45 AM | Comments (5) | TrackBack
June 25, 2008
Are GP gatekeepers a historical relic?
In an earlier post I raised the issue of the GP as the gatekeeper of primary health care. It was posed by stating the AMA's position, which is:
General practice is the gateway to allow patients enhanced access to other health professionals - including general practice nurses and allied health service providers such as physiotherapists and dieticians
I then asked why should the GP be the gateway to the health system for those consumers whose preference is to see a dietician, psychologist or a chiropractor? Why cannot we consumers see the latter health professionals direct? Isn't this a reasonable position when there is a shortage of GP's, especially in the outer suburbs of the metropolitan centres and regional Australia? AustraliaŌĆÖs health 2008 showed that the overall supply of GPs decreased by 9 per cent between 1997 and 2005.
The GP as gatekeeper has been one of the stumbling blocks upon which health reform has been resisted. The Rudd Government is trying to move this stumbling block to one side in order to make room to tackle the national GP shortage, which makes it difficult for Australians to access primary care. The aim is to give allied health health professionals (nurses and physiotherapists) access to funding under Medicare and the Pharmaceutical Benefits Scheme.
The response by the AMA is direct: patient care would be compromised if anyone without the all round expertise were made the first point of contact in the health system. In her National Press Club address Dr Capolingua, the President of the AMA, ridiculed the ALP's proposal for a "one-stop shop" health centre as a "myth", and said that this would result in the fragmentation of care. She spoke of a scenario where a patient has a brain tumour undiagnosed after going to a super clinic with a weight problem and being referred to a dietician and psychologist. She has also warned that the GP superclinics would put private GP's out of business.
Only 31 GP superclinics are proposed, they offer integrated multidisciplinary care, and are located in areas where it is difficult for families to access their local GP, and so they end up in their local hospital. So it is good health policy to turn to allied health professionals for primary care.
On the AMA's account GPs are the gatekeepers holding the gate open to facilitate access to the most appropriate specialist or allied health provider for each individual patient, and coordinating that care. Since GP's do not have expertise in non-drug care nor in mental health why should they coordinate that care as opposed to the suitably qualified non-medical health professional.
Posted by Gary Sauer-Thompson at 7:11 AM | Comments (20) | TrackBack
June 18, 2008
AMA makes its stand
I see that the AMA has come out fighting against the proposed extension by the Rudd Government of Medicare to nurses and allied health professionals (such as psychologists and physiotherapists) in response to the shortage of GPs. It is another plank in their resistance to reform as can be seen in campaigning against the government's GP Super Clinics and the doubling of the Medicare surcharge levy threshold.
The core bit in their latest media release, in association with other doctor organizations, states that the GovernmentŌĆÖs proposed National Primary Care Strategy should ensure that:
- Australians continue to have access to high-quality general practice services;
- General practices are given additional support to allow them to deliver more preventative health care services and tackle the growing burden of chronic disease;
- General practice is the gateway to allow patients enhanced access to other health professionals - including general practice nurses and allied health service providers such as physiotherapists and dieticians;
- Primary health care services in workforce shortage areas such as rural Australia are improved through incentives and assistance to get more general practitioners and primary health care teams in these parts of the country;
- General practice training opportunities and incentives are enhanced so that many of the new medical school graduates choose to enter general practice over the next few years.
Australians, it says, have confidence in their general practitioners having overall responsibility for their primary care needs and that the future of primary health care in Australia should build on this system not undermine it.
I've listed these points in the media release to show how much the AMA is in flight from reality. Two points show this. First, the AMA 's only solution to the lack of GP's in rural and regional Australia is for the commonwealth and state Government to provide incentives and assistance to GP's to get more general practitioners and primary health care teams in these parts of the country. But here already are health professionals there delivering primary care. So why not utilize them? Why not extend Medicare in these parts of Australia to help those who are sick and unwell. Why cannot patients be able to access Medicare-subsidised care without a referral from a GP?
So what does the AMA say in response?:
Reforms that do not support the important role of general practice will progressively erode the health systemŌĆÖs function, patients will experience more fragmented and uncoordinated health care, and primary health system costs will inexorably rise.
Note the phrase--'erode the health systems function'. It has already has been eroded. The reforms are addressing it.
Secondly, the AMA says:
General practice is the gateway to allow patients enhanced access to other health professionals - including general practice nurses and allied health service providers such as physiotherapists and dieticians
Why should the GP be the gateway for a consumer to see a dietician, psychologist or a chiropractor? Why cannot we see them direct?
These two points highlight how the AMA is simply protecting its turf --a demarcation dispute hidden by the rhetoric of public safety and quality health care.
Posted by Gary Sauer-Thompson at 6:49 AM | Comments (14) | TrackBack
June 12, 2008
medical politics
As we know health is back on the reform agenda --in terms of private health insurance and primary care in the context of an ageing population, the increasing incidence of chronic disease, national workforce shortages and ageing infrastructure.
Private health insurance continues to churn away under the surface as it irritates many because it props up the private health insurance industry. Kenneth Davidson in The Age addresses the issue of private health insurance. He says that the unstated policy of the Howard government was designed to prop up private health insurance and maximise the incomes of doctors at the expense of the public health system but not, as far as he is aware, the policy of the Rudd Government. He says:
But one thing is incontrovertible. The carrots and sticks didn't take the pressure off Medicare. In the situation where there is a shortage of GPs, specialists and nurses, a shift in funding away from public to private provision of health services will lead to a similar shift in health professionals.It follows that if the imposition of the 1% Medicare levy surcharge (and the 30% health insurance rebate) didn't take the pressure off Medicare and the public hospital system, reversing the surcharge (and the 30% rebate) won't cause a mass exit from private health insurance as has been predicted by the AMA and the private health insurance industry
Charles Livingstone, senior lecturer in the Department of Health Science at Monash University, says that what private health insurance does is help people jump the queue, as Howard government advertising highlighted. It does this by paying practitioners more in the private system, and exploiting the differential created between public sector rates of remuneration and those on offer in the private sector
What Davidson misses is that hospital care is not everything. Primary care is crucial, even if it is usually overrlooked. In primary care there is a shift towards opening up Medicare to nurses allied health professionals working in a team headed by a GP.That basically means the patient does not need to see the GP for health care. This way of addressing a chronic shortage of general practitioners will be opposed by the Australian Medical Association which has long-campaigned to maintain the monopoly of GPs in delivering primary health services in the name of quality and safety.
The proposed reforms does not mean that allied health professionals are accepted as primary care practitioners in their own right, even though people do see them independently of the GP. They can be seen as a step in this direction. We have a long way to go to break the monopoly of GP's in delivering primary health care services to allow allied health professionals to deliver primary health care.
Update
Davidson also misses the way health services in rural and regional Australia are being reformed with due to the pressures resulting from ageing population, the increasing incidence of chronic disease, national workforce shortages and ageing infrastructure. There is a greater shift to the hubs (hospitals) and spokes (primary care) model, greater co-ordination, better greater integration of services and an increased focus on community need. This means that the role of hospitals will change with an emphasis on upgrading several acute care regional general hospitals with the smaller country hospitals acting as feeders. The smaller hospitals will provide palliative care, primary health care, community based mental health, overnight and day surgery, rehabilitation etc.
Posted by Gary Sauer-Thompson at 8:29 AM | Comments (19) | TrackBack
June 5, 2008
health workforce
I was at a Health workforce forum in Sydney yesterday. It was early start late finish cos of planes and battling Sydney's gridlocked traffic in the wet.
The forum was run by reform minded bureaucrats under the auspices of CoAG. The political problem faced is this: the new investment in health workforce will not be enough to replace the baby boomer health workers. This shortage in supply is made worse by the increased demand on health services by an ageing population. Crunch time. State and federal budget budgets blow out from health care.

So what is to be done.That's what the various committees have been set up to future out and advise state and federal ministers. The forum was the bureaucrats reporting back to the various stakeholders on what had been achieved by them and obtaining feed back to what they were up to.
Public health services are in a very bad way in NSW because the previous Carr/Egan regime was obsessed by debt reduction and so they did not invest in health care --along with a lot of other infrastructure--for far too long. Now the Iemma/Costa regime is trying to buy its way out of trouble and they will go into debt to fund the infrastructure spending.
Hence the talk about co-operative federalism. How far Iemma + co support structural change iand system reform in the health system is unclear. The Health MInister talks in terms of innovation in service delivery and traditional responsibilities not being allowed to stand in the way but it is unclear what this means at a political level in NSW.
Posted by Gary Sauer-Thompson at 1:05 AM | Comments (1) | TrackBack
May 22, 2008
why subsidise private health insurance
One washup of the Swan budget is the health debate arising out of the changes to the Medicare Levy surcharge, which in effect reduced the tax on citizens that was then used to prop up the private health insurance industry. The Liberal Party's rhetoric is that reducing this tax is being done because the ALP hates private health insurance in the same deep way that they hate private education.
As pointed out in an "earlier post this debate is being framed by the vested interests of private health insurance as an issue about the public health system to avoid the question of subsidy of the private health funds. It also carefully avoids the significance of primary health care outside hospitals and the issue of whether the way we fund and organise primary care needs a major overhaul.
In his second post on changes to the Medicare levy threshold Tim Dunlop at Blogocracy says that he is very interested to hear some fact-based discussion about why the system of subsidy for private cover shouldŌĆöas the AMA, the Opposition and the health industry argueŌĆöremain pretty much unchanged. Facts are in short supply at this stage in the debate, but we can look at the arguments for why the private health industry needs to subsidised so heavily when a neo-liberal mode of governance is deeply opposed to government intervention in the market, celebrates lower taxes, and opposes subsidies and protection.
As Tim Dunlop says this is an industry that calls on the public purse in order to maintain their own profitability. Mike Steketee concurs in his op-ed in The Australian. The health funds, he says are propped up by so many government supports that their product is more accurately described as semi-private health insurance:
No other industry receives a 30 per cent government subsidy on the prices it charges: make that 35 per cent for premiums for members between 65 and 69 and 40 per cent for those 70 and over. The tax surcharge continues for income earners above the higher thresholds set in the budget, with the aim of pushing them into private insurance. There is the government-mandated 2 per cent a year increase in premiums for every year people delay taking out insurance after they turn 30. Then there is the discounted payment the health funds make for private patients treated in public hospitals. Finally, a tight web of regulation means competition between the funds is limited.
He then asks the right question: 'why in the name of rational economics should we be pouring vast amounts of taxpayers' money into an industry that is uncompetitive and provides a more expensive service?'
Steketee then lists the arguments in support of the subsidies. The first argument that he mentions is this
The argument goes that we need a vibrant private health sector because it offers choice to patients and keeps the public sector on its toes. But who is to say the ideal level of private health insurance is about 45 per cent of the population, as at present, rather than the 30 per cent it might fall to without enormous government subsidies?
The reason is that at 30 per cent the private health industry is not viable. It needs a certain mass and that is around 40%. So why do need to keep the industry viable? Shouldn't that be about offering good health products to attract consumers to buy the product in the marketplace. Why is this exception made to the way the market works?
This is where the second argument cuts in, and it is not an infant industry argument. Steketee says:
Private health insurance, say its supporters, takes pressure off public hospitals. But to the extent that is true, it comes at a cost. Doctors charge higher fees for private patients, who also are more likely to undergo more procedures and more expensive ones. This would not necessarily matter if the quality of medical care was better but the evidence on this is ambiguous. Nor would it matter if it did not involve large buckets of government money to private insurance. The 30 to 40 per cent rebate alone cost the federal budget $3.5 billion last financial year. In terms of its impact on health, much of it is wasted because it goes to people who had private health cover before the rebate was introduced and would keep it whether or not it was subsidised.
Steketee says that a much better use of the money would be to spend it on public hospitals or, for that matter, private hospitals. Steketee, like the other commentators, ignores the better option of investing money into revamping primary health care to keep people well and out of hospital. They debate is being conducted as if the network of diverse (medical and non-medical) primary care practices don't exist. It is this absence that gives an air of unreality to the debate about health care.
These are the only two arguments that Steketee mentions. The other argument is competition: the private health industry provides competition to the public health system and keeps the latter on its toes as well as offering choice. The problem here, as Alan Mitchell pointed out in yesterdays AFR, cost containment is the weak spot of Australia's private health insurance and fee-for-service medicine, and little is done to strengthen the discipline on costs. Inflation is actually built into the private health care system.
Steketee rightly points out that a major explanation for why the private funds struggle to keep their members is because they offer a poor product:
Out-of-pocket costs are the main reason people cite for giving up their membership. Understandably, they resent being rewarded for buying insurance by having to fork out extra money when they actually claim benefits. There has been a reduction in the number of private patients facing gap payments but after at least 15 years of trying to sort out this issue, more than 15 per cent of hospital services still involve a gap payment and one that is increasing.
They have no incentive for cost containment as they can keep increasing their premiums year by year above the inflation rate. Steketee says that The funds are not to blame: they are well aware of the damage gap payments cause to their business. But they often lack the clout to force doctors [specialists?] into agreements that guarantee no gaps and when they do succeed, the doctors [specialists?] can extract a hefty price.
Surely the larger funds with market power could extract more favourable deals from private hospitals and specialists? Secondly, the Rudd Government can put pressure on the private health funds by increasing the competitiveness of the public system by ensuring a cut in queues and increasing the quality of services. Thirdly, rather than providing ever more subsidies the Rudd Government should require the private health funds demand performance by cost containment by the use of case-mix funding by the services they private hospitals provide. This would put pressure on private hospitals with above average costs and encourage the private hospitals to specialize where they have cost advantage.
Posted by Gary Sauer-Thompson at 7:43 AM | Comments (6) | TrackBack
May 20, 2008
scaremongering on health care
There has been some debate in the media about the extent of the numbers dropping private health insurance as a result of the Rudd Government raising the threshold at which the Medicare surcharge levy cuts in ( now $100, 000 for singles and $150,000 for families). The threshold surcharge was introduced by the Howard government to push people into taking out private health insurance as they would have to pay the higher Medicare levy if they remained in the public system.
The private system has been supported by three policy props introduced in the 1990s by the Howard Government to stop the decline in private health insurance membership. These props were a tax surcharge of 1 per cent on top of the Medicare levy for those who do not have private health insurance, a 30 per cent government rebate of premiums for those who do, and age rating that progressively increases private health insurance premiums for those who enter the system after age 30.
The numbers leaving private health insurance would have been run by the computers in Finance, Treasury and Health and Ageing (in this case Treasury) as part of the budget process. That analysis is not for the public, or even opposition Senators, but the leaked figure from Treasury is 480,000 dropping out, with some projected government savings(estimated at $230 million) in terms of the 30 per cent government rebate. The leak from the work of Crosby-Textor to the Australian Health Insurance Association (AHIA) says that around 425,000 would leave. I donŌĆÖt know any other modeling or references that have been done on this. These figures are much lower than the 900,000 quoted by the Australian Health Insurance Association based on the private work of Pricewaterhousecoopers.
I donŌĆÖt buy the argument that dropping out of the private health insurance necessarily leads to increased queues at public hospitals causing collapse etc. Most of those dropping out ----cos itŌĆÖs a bad and expensive product---are young and healthy and so it will not make much difference to the public health system. Those dropping out will turn to primary care practices in order to stay well and out of hospital.
Those arguing the big increase in public hospitals that are on their knees (the increased strain on the public health system will be a huge burden on the rest of the population, reducing our public health system to a third world one) reduce health to hospitals and ignore the significant role played by primary care in keeping people out of hospital. They cover this flaw with their talk about the ALP's ideology. Its all ideology for ideology's sake. No mention is made that it raising the threshold at which the Medicare surcharge levy cuts in is a tax cut that empowers consumers and enables them to decide how they spend their money on health.
Sure, private health premiums will rise (health funds will lose profits from drop in the numbers of fit and healthy singles). The estimate is around 5%. That means the private health funds need to find ways to increase their membership. They could, for instance, develop wellness packages (chiro, gym, nutritionist, physio, massage, psychologist) etc to entice consumer singles to buy their product, rather than relying on state coercion and big subsidies to keep them viable and profitable. This is the marketplace after all, and that means value for money.
What we are currently witnessing is scaremongering.---bully boys pressing the fear button etc----by the Australian Health Insurance Association. No doubt the private health industry will also try to get its hands on of the Rudd Government's flagship $10 billion health infrastructure fund, as these funds will go towards hospital wards as well as medical facilities, technology and projects. That money should be for public hospitals not private ones.
Update: 21 May
The conflict over numbers leaving the private health system as a result of the Rudd Government raising the threshold at which the Medicare surcharge levy cuts in continues with the AMA now weighing into the debate. A report commissioned by the Australian Medical Association (AMA) from Access Economics says that to achieve Treasury's projected savings of $230 million 800,000 people would have to abandon private cover by July. Why start there? Maybe Treasury's estimate of the savings is wrong?
The AMA is spelling out how people will leave---slowly----and it is warning of increased pressure on public hospital bringing them to their knees. The AMA can't argue that it is young people that will be pulling out of health insurance making it more expensive, and argue that those same people are the ones that will overburden our public hospitals.How come the singles won't be visiting their local friendly GP instead of going to the emergency department of the public hospital? Doesn't the GP provide high quality health care?
So the AMA is defending a public subsidy of private health insurance through a special tax on consumers. The specialists in the private hospital system (for whom the AMA speaks) want a special tax to keep their money rolling. Amazing. What ever happened to the principle of the Liberal and free market types that lower taxes are good and higher taxes are bad? Conveniently forgotten when it comes to the private health industry it would seem.
This is yet another indication that the AMA is opposing health reform that addresses equity issues.
Posted by Gary Sauer-Thompson at 6:56 AM | Comments (11) | TrackBack
May 19, 2008
mental health
In an op-ed in The Australian Ross Fitzgerald says that:
For those concerned about mental health, the Rudd-Swan federal budget is a huge disappointment. The only new measure is the allocation of $2.4 million over three years to establish a national advisory council on mental health to co-ordinate commonwealth, state and territory services to people with a mental illness, but there are no new funds for this or other services.
Yet although about 20 per cent of the population have significant mental health problems, about half do not receive adequate treatment. This especially applies to those with a dual diagnosis.
Dual-diagnosis patients have a psychiatric illness such as schizophrenia, serious depression or bipolar disorders, coupled with a major problem with substance abuse. These patients are often the most difficult to treat because substance abuse interferes with psychological and pharmacological treatments. Specialists in the field estimate that, in the wider community, 50 per cent to 60 per cent of those using chronic and acute mental health services in Australia have substance abuse disorders as well.
The public health system is poorly resourced to treat these people, due to the emphasis on quick turnaround in our public hospitals. During the last years of the Howard government, there was increased access to psychologists and social workers through Medicare and the provision of mental health nurses for psychiatrists and general practitioners.
Posted by Gary Sauer-Thompson at 8:30 AM | Comments (3) | TrackBack
May 13, 2008
Roxon's health budget
I didn't see Wayne Swan's budget speech. I was in a health budget lockup in Woden in Canberra and I only saw the beginning of Swan's flat and nervous speech at the end of the tedious briefing. I decided that doing a bit of networking was more important than listening to Swan's baptism as Treasurer helping us deal with uncertain economic times. I'd heard too much from the Rudd Government media management machine "behind the scenes" that produces all those leaks and spin. The budget speech was a non-event.
The health section of the budget suggested that the reform is going to be modest---cautious reform step by cautious reform step. Nothing to rock the boat--- no major redirection under a new government. The centrepiece of the health budget is the $10 billion dollars from the huge Budget surplus ($21 billion) being ploughed back into Australia's health infrastructure under a new fund. This fund, which builds on Costello's ideas, was forgotten by Jane Hailton, the Health Department Secretary, and only recalled at the last minute. Instead we got minutiae in the presentation from the various departmental secretaries that downplayed the cuts in spending in mental health especially, without any narrative of what the health budget was trying to do. I just cannot see the Department of Health and Ageing driving reform.
The Health and Hospital Fund is to be to be managed by the Future Fund. No mention was made of a COAG Reform Fund, which will also be set up to channel reform-related payments to the States.The establishment of the health and hospital funds,(along with infrastructure, education funds) gives a good sense of the nation-building intent over the course of several Parliamentary terms.
There was a push towards preventative care (alcohol, smoking and drugs) and cuts to programs without wielding the meataxe---there's a sense of the Razor Gang going line by line through the spending inherited from the Howard Government----and it meet all its election commitments in this Budget in terms of increased funding for hospitals and GP Superclinics. There was the updating of the Medicare surcharge levy:---raising the threshold ($100,0000 for individuals and $150 000 for families) for people who choose not to take out private health insurance. Is that an indication of reform intent re the public/private health mix.
The health budget indicates that Tanner and Swan have cut spending but not so savagely that the budget will not continue to grow slightly in real terms. The savage attack on spending promised by the Government over summer to fight out of control inflation was rhetoric. What has been done----a reduction in real spending growth to 1.1% from the 5%+ growth of CostelloŌĆÖs last Budget---- is probably enough to keep the Reserve Bank from increasing interest rates. The Finance Minister has found $2 billion more in savings than Swan and Rudd are spending.
Swan and Tanner reconcile the need for fiscal restraint to fight inflation while fulfilling the GovernmentŌĆÖs election promises and not crunching the economy so hard that it risks exacerbating the coming slowdown. So it is politically astute.
I saw Peter Dutton, the Opposition Finance spokesperson, on Lateline saying that this is a true Labor budget because there's high spending, there is high taxation. He gave every impression of not knowing what he was talking about as he tried to spin a line----the Rudd Government is socialist! The implication was "politics of envy"--- soaking the rich to give to the poor. The budget's big tax cuts-- copied from the Liberals during the election--- does not support that interpretation at all.
What Dutton didn't, or couldn't, say was that the tax cuts ($31billion) are clearly inflationary in an economy that is still at full stretch. Much of them will be spent. They are the centrepiece of the Budget, and in the last couple of months of Government decision making the Razor Gang been running trying to undo the effect of those tax cuts by cutting government spending. Chris Richardson from Access Economics says:
I fear that inflation will be worse than Treasury hopes. Remember, an absolute torrent of money is about to be dropped on Australia's economy. It's not just the commodity boom's continuing, it is accelerating, and this is the biggest set of risks we've had in this inflation challenge so far. The Budget helps, but whether it's helped enough, not clear.
He says that though all the headlines are about US recession, market meltdown, highest interest rates. The biggest thing happening to the Australian economy is the massive jump in coal and iron ore revenue.
There's a good position for the Coalition to argue from. Much better than Turnbull's "what inflation?" rhetoric that is at adds with the analyses of the Reserve Bank and Treasury; or is his subsequent defence of big centralized government with his repeated warnings against substantial spending cuts --wielding the machete and inflicting lots of pain ---at a time of a global economic downturn.
Posted by Gary Sauer-Thompson at 9:31 PM | Comments (5) | TrackBack
May 9, 2008
the limits of health prevention
Jeremy Sammut, a research fellow at the Centre for Independent Studies, has an op-ed in The Australian on health prevention, lifestyle illness and wellness tha tis based on his recent monographThe False Promise of GP Super Clinics, Part 1: Preventive Care He says that Australian governments have told us to quit smoking, eat moderately and exercise regularly, most memorably through the Life! Be In It campaign. We have listened, up to a point at least, and the easy prevention work has now been accomplished. He adds:
Many middle-class people are converts to the wellness cult: they have stopped smoking, improved their diet and started to exercise. But many others, particularly those on lower incomes, prefer to live for the day and have ignored the healthy lifestyle message. Recent reports on public health policy in Britain and Australia found that despite decades of spending on prevention programs, levels of physical activity have not increased and obesity levels have shot up. Obesity-related chronic disease already puts pressure on the health system and it will accentuate the challenges we face as the population ages.
Prevention hasn't worked, he says, because however intensively the health lifestyle message is pushed, it comes down to individuals to have the will, self-discipline and impulse control to change longstanding behaviours that are often pleasurable. As international studies have found, the main reason anti-obesity initiatives have failed is that many people find it difficult to sustain lifestyle modifications for long periods.
Okay, that is pretty right. So where to next? What policy options do we have to address this?
Sammut rejects government intervention as it is paternalistic and an example of the nanny state. He argues that the Rudd Government holds that it is the government, rather than the individual, that the experts deem responsible for obesity, because it has not done enough to force people to drop their hamburgers and get off the couch. Their argument is interpreted thus:
Obesity has been redefined as an epidemic, as if victims passively contract it (infected, of course, by wicked and coercive fast-food advertising). As the victims of this epidemic are concentrated in lower-income groups, obesity has also been classified as health inequality, which makes it a social problem. The failure to curb obesity demonstrates is how the system failed to provide help to turn knowledge into practice. So-called ordinary Australians therefore need Medicare-funded preventive health care, of course, because unless the government was prepared to help them, how could they be expected to take care of their own health.
He says that cheered on by the experts, the Rudd Government is determined to unfurl a new range of preventive policies to try to contain the future cost of Medicare.
The word 'force' is misleading in this context given that the health prevention has been one of persuasion. So is the idea of liberal subjects seen as passive victims of an evil fast food industry. No mention is made of fast food being an unhealthy product.
What is the alternative? Sammut turns to the individual:
But the evidence suggests the Government's policies won't work. It should let ordinary Australians be and help ordinary taxpayers instead. Millions of taxpayers' dollars are already wasted every year preaching the virtues of brown bread, wheatgrass juice and jogging to those who won't be converted.
Letting them be rather than helping them is deemed a good policy, even though they are unwell and seeking help in clinics? "Converted' is the wrong word. This implies that wellness in the form of healthy functioning is a religious cult and not a form of primary care.
Posted by Gary Sauer-Thompson at 6:49 AM | Comments (4) | TrackBack
April 29, 2008
Alcopop tax + health prevention
I see that the Rudd Government has placed a heavy tax on alcopops, the ready mix alcoholic drink that tastes like soft drink and is primarily marketed to teenage women. The excise on pre-mixed drinks, or alcopops, almost doubled on Saturday, from $39 a litre of pure alcohol to $67. The change means the price of alcopops such as Bacardi Breezers and Vodka Cruisers will increase by between 30c and $1.30 a bottle, depending on the alcohol content.
This kind of policy is in the tradition of taxing cigarettes to help reduce their consumption. No doubt the libertarians will mutter about the nanny state and individual freedom and teenagers will shift their alcohol consumption back to beer and wine. No doubt the AFR will do its populist sneer routine whilst going about competition, productivity, infrastructure and tax reform.
 Bill Leak
Bill Leak
The justification for the tax rise is that a "significant proportion" of the revenue would be directed to the new black in health funding, preventative health programs. So something has come out of the 2020 Summit, in which each section had to come up with one big idea, and three policy ideas, including one that came at no cost.
This does help to shift the debate away from the medical model and hospitals to health and prevention. What we don't want is the money being spent on chronic diseases in public hospitals as the aim is to keep people out of hospitals by keeping them well.
Will junk food be next? We do need to make healthy food choices easy and this could include having a single food labelling system and food component labelling system; having healthy food choices at child care settings, schools, sporting venues and workplaces;regulating food marketing to children (banning junk food advertising and marketing through internet sites).
Update: 30 April
This cartoon represents the two aspects of the tax on alcopops. Most of the libertarian emphasis is on the tax /revenue raising side withe the public good of health prevention being pushed into the background.
 Moir
Moir
The libertarians in Australia are primarily consequentionalists about individual liberty ----liberty is conducive to good consequences. A morally right action is one that produces a good outcome, or consequence. Since the tax is an imposition on individual liberty, it is bad. Limited government is good as it gives more space to sovereign individuals to exercise their liberty. The nanny state is bad because it impinges on individual liberty.
Posted by Gary Sauer-Thompson at 5:17 AM | Comments (13) | TrackBack
April 20, 2008
2020 Summit: health
A tax on junk food, alcohol and tobacco to fund a national preventative health agency and programs to keep people healthy is the big idea of the by health experts at the 2020 summit. They stressed the need for a major boost in the share of the health dollar spent on keeping people out of hospitals, but to make the idea cost neutral, they opted to pass on the cost to consumers of products that unduly added to the burden of obesity, cancer, diabetes and injury ŌĆō drink, fatty foods and cigarettes.
 Spooner
Spooner
Is that an illustration that the summit was about more about symbolism, less about substance? Or an example that the gathering was dominated by inner-city dwellers, many of whom have had a public platform to sprout their ideas ŌĆ£either in academic journals, parliament or newspaper columns. Was this an example of the ideas that indicated that the Summit was a gathering of the inexpert, the unqualified and the inexperienced?
Posted by Gary Sauer-Thompson at 9:09 PM | Comments (8) | TrackBack
March 27, 2008
Evaluating CoAG reforms
So what do we make of CoAG's Adelaide agreements on health? Is it historic? Hardly. Public hospitals will receive an extra $1 billion after state governments warned Rudd they could not they could not meet his challenge to lift their health performance on current funding levels.
That extra interim funding of $1billion - $500 million in new money and another $500 million over last year's funding levels to match rising inflation---restores some of the reduction in funding under the Howard regime.What had been for years had been a 50-50 funding deal between states and commonwealth had turned into a 60-40 deal under Howard.
However, the new money will not be subject to strict performance reporting levels promised by the Prime Minister to improve hospital efficiency by making states more accountable for how they spend public money. So it is just more money for the states with no strings attached. The states only agreed to work creating performance benchmarks across all areas in which they receive common wealth grants. Why not performance benchmarks for state health funding as well? The states appear to interested in wanting to get as much money out of the Commonwealth as possible and not in a fundamental redesign of AustraliaŌĆÖs health "system".
Will this kind of accountability be argued for by the newly created National Health and Hospitals Reform Commission? We will have to wait and see. The Commission has wide terms of reference though.
Is the Adelaide health agreement a step in the reform process that was blocked by the previous Howard Government ?
The National Registration and Accreditation scheme went through, despite the AMA's objections. The details are unclear. That reform has been a long time coming and it is long overdue. But it's no great reform shift. It is even unclear how far the movement from self-regulation has been or how it is connected to other reforms.
The workforce plan to create 50,000 health training places for enrolled nurses, dental health workers, allied health professionals, ambulance officers and Aboriginal health workers was agreed to Such a contrast to the Howard Government focus on solely creating more doctors, and it is a belated response to health workforce crisis that has been building since the 1990s.
Will there be problem filling the training places? Are people attracted to this kind of work? Will the states boost the wages of nurses in the public health system to attract the nurses? Unlikely. We seem to have disjointed incrementalism, a process where policy initiatives are made in isolation rather than against a background of a broad strategic vision for the system.
The implication is that this CoAG meeting did not have a reform agenda that actually delivers better health outcomes. Maybe the Rudd Government is awaiting the work of the National Health and Hospitals Reform Commission key issues of chronic disease, ageing of the population and rising health costs).These will require solutions based on workforce reform and restructure, including clinical role substitution and a greater focus on multi-disciplinary care, the exclusion of experts from the non-medical health professions.
Will the Commission find ways to overcome the power barrier to the identification of innovative approaches that don't place doctors at the centre of the health system?
Posted by Gary Sauer-Thompson at 9:12 AM | Comments (3) | TrackBack
March 25, 2008
CoAG + health reform
CoAG meets in Adelaide tomorrow and it appears that the Rudd Government is using this as a way of governing the country and pushing the modernizing agenda --to make CoAG a reform workhorse. The suggestion to widen the CoAG agenda to include financial regulation of margin lending, mortgage brokering and non-bank lending indicates that. It's about time that kind of national financial regulation happened.
Is CoAG picking up on the older National Reform Agenda on which little progress had been made under the Howard Regime? Is the older strategy of incentive payments pioneered under National Competition Policy going to be used?
Health will also be on the agenda. The signs indicate that the commonwealth's emphasis will be for more accountability from the states on health, insisting they accept tough performance reporting requirements to demonstrate efficiency in spending commonwealth money. No doubt the NSW Lemma Government will continue to resist with spurious arguments.
The signs are there that here will be a push of a national registration and accreditation scheme. The AMA has come out in opposition as is expected. They have a history of opposing major reform that undercuts their power as the gatekeepers of the health system. That power must be defended at all costs. It is a totemic political issue.
Some of the proposed reforms are long overdue such as paying the states to clear the nation's hospital wards of 2000 elderly people who are occupying valuable bed-space but who should be in nursing homes and nationally harmonized occupational health and safety legislation.
Posted by Gary Sauer-Thompson at 7:49 AM | Comments (6) | TrackBack
March 10, 2008
Rudd Labor, health reform, modernization
Nicola Roxon, the federal health Minister, talks in terms of root and branch reform of health care. Kevin Rudd, the Prime Minister, talks in terms of a hefty injection of federal money and a set of selective federal performance targets bringing the state's performance of their public hospitals up to a level where they are out of the headlines. The inference from Rudd is that he is not embarking on a basic structural reform.
Since Wayne Swan, the Treasurer, and Lindsay Tanner, the Finance Minister, talk nonstop about cutting back the federal budget and government spending to fight the inflation monster, I cannot see how that fiscal conservatism will lead to the 'root and branch' reform that Roxon is talking about. From what I can judge there is not going to be much 'root and branch' reform to provide better health care services in the first term of office.
So what then of Rudd Labor's reforming, modernising programme? What does it consist in? What is it trying to achieve? Are there dominant and subaltern elements of Rudd Labor's reforming, modernizing programme. Is the conflict between the two going to be managed by spin?
Will the modernising centre-right cause Rudd Labor to become the 'great moving right show' that pre-empts any substantive move of the government in a leftward direction. The left's old welfare state positions have been marginalised.The traditional left binary, antagonistic vision of an alternative future based on public health (modelled on the NHS) that is opposed to private health and the market has little credibility, and its appeal is now residual, a demand for recognition of what seems to be a social force in decline.
On the other hand the strategy by the right to ŌĆśroll backŌĆÖ these gains (via ŌĆśmodernisationŌĆÖ, ŌĆśflexibilisationŌĆÖ, and ŌĆśreformŌĆÖ) continue to make up the main agenda of democratic politics in Australia; but this remains stalemated after the last election when the Australia electorates do not vote for a worsening of their own conditions of life.
Posted by Gary Sauer-Thompson at 6:08 PM | Comments (9) | TrackBack
March 9, 2008
medical self-regulation has failed
It bothers me that state governments do little about Medical Boards that fail to regulate the medical profession to ensure public safety and quality of care. The regulatory medical boards are simply not doing enough to protect patients from the adverse events caused by incompetent, predatory, drug-dependent and unstable doctors.
So we have the well known cases of Dr. Death at Bundaberg Base Hospital in Queensland, the "butcher of Bega"--Graeme Stephen Reeves---in NSW; and in Victoria, and the dermatologist Dr David Wee Kin Tong. In all three, the regulatory medical boards, 'the watchdogs', have failed dismally in their duty to protect the public, and they have evaded their responsibility to ensure public safety.
 Greg Roberts
Greg Roberts
Self regulation has long been argued by the medical profession in particular as being the preferred method of maintaining standards of care. In the case of the medical profession, this has largely been achieved through the learned medical colleges. The above examples are recent examples of the failure of medical self regulation
There is a convention in the medical culture that the medical regulatory authorities, professional colleagues and administrators overlook adverse events medical mistakes and complaints that medical practitioners were acting outside the bounds of appropriate professional conduct.The medical mistakes remain a professional matter and the medical disasters are covered them up.
As The Age editorial says in relation to the Reeves ruining the lives of scores of women by mutilating their genital organs with surgical procedures that were usually botched and often unnecessary:
But even worse than the actions of one criminally careless and dangerously deluded doctor is the fact that a brotherhood of fellow practitioners failed to stop him. In fact, it seems that the quaint, cosy system of self-regulation Australian doctors enjoy actually helped to bury the truth about the damage Reeves inflicted on women placed in his care.Other surgeons called in to attempt to repair Reeves' botched operations knew who was responsible but it appears that they ŌĆö and other hospital staff ŌĆö preferred to observe a code of silence of the sort usually associated with organised crime: an appalling silence that is completely at odds with the Hippocratic oath doctors swear but which too many of them seem to regard as a relic.
The editorial ends by saying that it is vital that a fearless, independent regulator has the power to investigate doctors who abuse patients' trust. On this, physicians cannot be expected to heal themselves. Governments must act.
Posted by Gary Sauer-Thompson at 10:49 AM | Comments (8) | TrackBack
February 29, 2008
health in the headlines
Whilst the health ministers meet to discuss the new healthcare agreements Morris Lemma, the Premier of NSW, says that people in NSW is trust their own experience over hysterical headlines. And their experience is of a health service system that is making real progress, a government that is listening to the people who gave the Lemma government a mandate to make changes, and that they can trust Lemma + Co to continue to focus on improving services for families.
 Alan Moir
Alan Moir
Others argue that we live in a culture of complaint and there is no finer terrain for indignation, loathing and strident sanctimony than the embattled field of health care, despite the fact we are living longer, better and easier, constantly benefiting from advances in surgical science.
The states want an extra $3 billion a year over the next five years to address what they say was a funding shortfall under the previous government.There is also disagreement over what conditions the Commonwealth might attach to any funding to drive reform.
George Jelinek addresses the issues behind the headlines in The Age. He says that for too long we have denied that there is anything wrong with the health system and that there is a need for an open acknowledgement that these problems exist.
Our complex health system is under enormous pressure and these failures happen at the fault lines. At the heart of the problem are the twin pressures generated by a decrease in capacity because of the progressive reduction in the number of inpatient beds in our hospitals, and the increase in demand caused by a pandemic of chronic illness because of unhealthy lifestyles.
So what can we do?
On the demand side, it is time we as a community addressed the growing problem of unhealthy lifestyles. Our reliance on medical care to undo problems once they have developed will be unsustainable as the projected increase in chronic conditions occurs. Our reliance on pharmaceuticals is proving enormously costly to our community and mostly they don't resolve the problems anyway. Prevention is our most effective weapon. Healthy eating, exercise and finding some balance in work and leisure will, in the long-term deliver better results. We need to increase funding for public health programs. We need to promote wellness as an important aim, not just absence of disease. On the capacity side, we have gone too far with rationalising hospital bed numbers. We urgently need more hospital beds, and soon. And we urgently need more alternatives to hospital care. Hospital in the home programs need support and we need many more aged care places.
Posted by Gary Sauer-Thompson at 6:36 AM | TrackBack
February 26, 2008
health reform
Nicola Roxon, the federal Heath Minister, says the Commonwealth will not follow through with a two-year deadline to take over state hospitals across Australia if genuine reform can be delivered through negotiation.
We don't have any intention to take over the hospital system if we can get that sort of reform by negotiations with the states. Of course, the states want more money into the system and, of course, that is something we are prepared to consider. But we are not prepared to consider it as a blank cheque
Roxon warned that hospital funding is a ŌĆ£two way streetŌĆØand that the new reform commission announced yesterday to develop long-term solutions to health funding was designed to end the blame game between the states. It was also designed to provide a blueprint for a health and hospital system capable of dealing with the challenges of the 21st century.
The Rudd Government has knocked back a recent move by the states--led by the NSW-- for more no-strings attached heath funding
Posted by Gary Sauer-Thompson at 10:13 AM | Comments (4) | TrackBack
February 7, 2008
hospital reform
John Dwyer, in his op-ed in the Sydney Morning Herald--- Hospitals' health depends on reform - and dollars ---argues that the the inadequacies, and solutions, of NSW hospital system are obvious. On the problem side he says that though the vast majority of patients seeking help from our public hospitals receive a high standard of care, the incidence of misadventure, and the inequity that results when hospital services are rationed, are unacceptable.
These nationwide problems are a product of a work force crisis, (we have trained too few clinicians), increasing demand for hospital services from ever sicker patients (public hospital admissions increase by 2 per cent a year) and episodes where the clinical needs of a patient are not met by skilled staff....Each evening many hospitals have staff phoning medical agencies frantically competing for doctors who might help them out during the coming night. It is a lottery in which the doctor you "win" may or may not have the experience needed for the tasks required.
And the solution?
An individual hospital should be an invaluable asset for a "networked" hospital system with the services it offers and, equally important, does not offer, based on its ability to guarantee quality and safety. Role delineation is essential.Not all emergency departments are equal. Some should be rebadged as acute care centres and their capabilities explained to the public. Small hospitals near each other should act as "one hospital" on two sites offering excellence at both, but not duplication of services.He says that nurses, allied health staff and doctors are devoted to the system but feel disenfranchised. So upfront bonuses may attract nurses back to public hospitals. But unless more flexible working conditions, support and mentoring replace bullying and excessive work loads, retention will remain a major issue.
And:
We must follow international trends and focus on disease prevention, the maintenance of wellness, and the earlier diagnosis and treatment of potentially chronic diseases.The states must introduce new models of primary and community care. The most important reform is to build integrated clinical teams around general practitioners so doctors can care for those now being sent to hospital.
Posted by Gary Sauer-Thompson at 8:22 AM | Comments (3) | TrackBack
January 31, 2008
hospital care: pinpointing the problems
A report on government services by the Productivity Commission reveals that state and territory spending on healthcare grew by an average of 6.2 per cent annually in the decade to 2005-06, whilst commonwealth spending grew by an average of only 4.9 per cent.
And while the states have directed increased funding to public hospitals, the commission says a "significant factor" in the commonwealth's extra spending has been its support for the private system, via the 30 per cent rebate on private health insurance premiums. As a result, while overall government spending on public hospitals grew by an average of 7.9per cent annually in the decade to 2005-06, average spending on private hospitals grew by 25 per cent. Another indication of the development of a two tiered health system?
The figures confirm a report released last October by the Australian Institute of Health and Welfare that showed the federal government share of public hospital funding fell from 45 per cent to 41 per cent between 1995-96 and 2005-06, while the states' share rose from 46 per cent to 51 per cent.
However, we still have no way to compare hospitals or hospital systems in, and between, the states. So it is difficult to pinpoint what is working and what isn't working. So there needs to be a single set of data for private and public hospitals to pinpoint the problems.
Posted by Gary Sauer-Thompson at 10:11 AM | TrackBack
January 22, 2008
a two tiered health system?
A key question in health policy is whether Australia's public health system can deliver safe and good hospital service given the current hospital structure and imposed budget constraints? Bundaberg, with its deaths and injuries, implies no. The Labor governments, state and federal, say yes, despite the shortages of hospital beds, shortages of doctors and nurses, the lack of funding for primary care. Public health, they say is now commonwealth as well as a state issue and co-operative federalism will ensure adequate patient health and safety.
It is a good question to ask in the light of the forthcoming Australian health care agreements. As Geoff Davies pointed out in an op-ed in The Australian on January 16 ('Patients risk death in our sick hospitals') these agreements:
are based on the assumption that all all Australians, irrespective of wealth, are entitled to free hospital care and treatment, including operative treatment; not just emergency care and treatment, but also elective procedures. What has not been considered, and what politicians have so far been reluctant to consider, is whether that assumption is a realistic one.
The quick and dirty response is that under a neo-liberal mode of governance, it is not a realistic assumption. A two tiered health system will develop as it has happened in education with its dual private and public systems. We already have a public and private health care system with the public one starved of funds under the Howard regime.
Geoff Davies acknowledges this possibility:
It is possible that, in the end, the only realistic choice may be between, on the one hand, a system that provides can provide free hospital care and treatment of all kinds to all people, but only inadequately seriously risking patient health and safety; and, on the other hand, one which can provide a safe and adequate system but not to all categories of people or not to of all services presently promised. But the possibility of that choice is open that politicians have, so far refused to confront.
Have they? Haven't we by default actually got the former kind of health system? The services are limited and rationed, and as adverse events in our public hospitals is the norm, this health care is unsafe and inadequate. What hasn't happened is politicians publicly admitting that the system cannot provide free health care delivered safely and adequately, and that they have failed to provided the resources to ensure a safe and adequate free public hospital system.
Posted by Gary Sauer-Thompson at 9:02 AM | Comments (14) | TrackBack
December 19, 2007
CoAG + health reform
The first Council of Australian Government's (CoAG) meeting under the new Rudd Government will be held this week in Melbourne on December 20. It will be the first CoAG meeting in which wall-to-wall Labor governments have sat down to hammer out a national reform agenda that died in the final years of the Howard Government.
It comes amid promises from the ALP that a new federal-state compact will be forged, leading to fundamental changes in the way Canberra and the states deliver services. Will this happen?

Alan Moir
The December CoAG meeting agenda focuses on health, education, climate change, housing , infrastructure and indigenous affairs. It promises to usher in an era of co-operative federalism. Co-operative federalism aims to to end what the ALP has called ŌĆ£the blame gameŌĆØ between the federal and provincial levels of government around health care. Can it be delivered?
It aims to do this through implementing Labor's election commitments on elective surgery waiting lists, the provision of aged care beds and a public dental program. These would constitute agenda item one for the commonwealth and the states and territories. However the states could not agree on an agenda and it has been entirely set by the Prime Minister.
I have not seen the point by point negotiating strategy contained in the high level policy papers, but the following information is in the public domain. It is stated that this COAG meeting will be more of a strategic discussion to outline a program of work for 2008, rather than aim to produce a policy agreement in these areas on day one.
Health care is the no I priority and it is understand thus:
1. The most immediate task is spend $100 million to remove the entire backlog of about 25,000 peoople who have spend longer on elective surgery waiting lists than the clinically recommended time.
Two strategies have been proposed to deal do this. First, surgical staff would be paid to conduct more operations outside normal hours---such as at night and over the weekend. And second, private hospitals would be contracted to help clear the backlog. Workforce problems are envisaged.
2. CoAG also needs to agree on how to implement the $300 million four year plan to provide competition policy-style dividend payments to the states to reward them for completing surgery within the clinically recommended time.
3. Another of CoAG's tasks is to set up the National Health and Hospitals Reform Commission. This body will set guidelines on how the performance of public hospitals can be judged.In the election Labor promised performance benchmarks for state and territory hospitals, and that if there is not improvement with 18 months, Rudd would propose constitutional referendum in 2010 giving the federal Government control of the nationŌĆÖs 758 public hospitals.
4. The other issues are spending more on aged care, boosting dental programs and preventative care, as well as cutting out duplication. It is not clear what spending more on aged care and boosting preventative care means.
The latter seems to involve GP Super Clinics in different suburbs. Labor's GP Super Clinic funding means that GPs will be co-located with other primary care services to provide more convenient and accessible health care services. They are expected to include privately practising GPs, a range of allied health services such as physiotherapy and podiatry, mental health services including counselling; and dental services.
Ken Baxter, writing in the AFR, says that a key problem in delivering the reform agenda is the lack of capacity of the state ministers and their supporting departmental officials in key areas to lead the policy debates rather than protect the status quo. Victoria is the exception to the state's public services being depleted of rigorous policy people or becoming highly politicized. It is the commonwealth's public service that has retained the intellectual rigor that has declined in the states.
Posted by Gary Sauer-Thompson at 2:44 AM | TrackBack
November 23, 2007
mental health crisis
Larry Hermann, a psychiatrist has an op-ed in The Age entitled Mental health system in crisis, that goes behind the slogans, headlines and the focus group words:
It is well known that mental health services have been underfunded for many years; not only crisis community teams but the whole public mental health system. Community treatment teams are not the issue; their dilemmas are symptomatic of not only long-term underfunding, but an ever diminishing workforce of expert staff. There simply aren't enough expert providers in mental health, both public and private, and never have been.
That's the description. What to do? What can be done? What could be done? Hermann adds:
My colleagues and I lament at the dumbing down of mental health expertise, which is only becoming ever more tangible....Governments, but no more so the current one, have for some time been introducing methods and policies to allow lesser trained personnel take over what used to be the domain of expert providers. No one would argue that it is absurd to suggest that surgery should be performed by anyone other than a surgeon. Yet in mental health it is increasingly common to see complex patient treatments occurring at the hands of inadequately trained staff.
Hermann includes psychiatrists in this as he refers to the common perception of psychiatrists as prescribe medications and out sourcing a complex level of their own expertise, i.e. psychological therapies, to others.
Hermann's solution is limited---it is for highly skilled clinicians to reclaim holistic and direct treatments of patients. But there are so few psychiatrists or even psychologists. Workforce shortages hit access hard in mental health as well as physical health.
Posted by Gary Sauer-Thompson at 6:05 AM | Comments (1) | TrackBack
November 2, 2007
health reform
Improved after-hours healthcare---ie., after-hours GP services--- is an important policy step and both parties have embraced it. It deals with an equity issue---proving after hours access for the working class who want to see doctors and so ease the burden on the hospitals.
Larger problems face both parties' plans, in particular the medical workforce shortage, which means any new centres will inevitably struggle to find staff. So what is needed is a national strategic health plan. However, Abbott, and the Howard Government don't see the need for health reform, and are they content to merely increase the number of Medicare items. So the states are pushing ahead their strategic planning and reforms on their own and leaving the Commonwealth isolated.
Posted by Gary Sauer-Thompson at 7:31 AM | Comments (4) | TrackBack
November 1, 2007
tax cuts v better health care
The Commonwealth Government appears unlikely to take full control of the Mersey hospital until after the federal election due to a medical registration bungle.Then we have a spat that played out on ABC Radio talkback on Tuesday morning between Tony Abbott, the commonwealth Minister of Health and Ageing and Lara Giddings, the Tasmanian Minister of Health over who is lying.
Todays Advocate editorial says:
..the Federal GovernmentŌĆÖs attitude was to seize the Mersey and worry about the detail later. It never consulted its own health department, bothered to find out how much it would cost, or tell the State Government about its plans ŌĆ” the ad hoc, often chaotic way this thing has been handled at times by the Feds smacks of political expediency of the worst kind.
This takeover was meant to a vote winner and the solution to the public hospital crisis, not just a means to hold the marginal seat of Braddon.

Sharpe
In the meantime we have the background debate between the budget surpluses being returned as tax cuts or invested in better health services. It's an odd debate since a substantial majority of Australians would prefer more goods and services from government, rather than personal tax cuts.
Jack Waterford, writing in the Canberra Times, points to ideology:
The cult of tax cuts, which began in the late 1980s, coincided with a general decline in public confidence in the capacity of the Government to change society for the better. It developed, reasonably enough, into a demand for greater choice in how services were taken up.
Posted by Gary Sauer-Thompson at 12:51 PM | Comments (7) | TrackBack
October 20, 2007
public hospitals in crisis
The Sydney Morning Herald reports another adverse event at Sydney's Royal North Shore Hospital---a patient with a serious spinal injury could not be operated on for five days due to a lack of staff and no available intensive care bed.

Alan Moir
Associate Professor Bill Sears said that it was a frequent occurrence that patients needing vital surgery were put at risk because they were made to wait due to a lack of intensive care beds. "It's a crisis. The hospital is a basket case"
Sears added that:
People just don't understand how seriously run-down Royal North Shore is. It's terrible. I've worked there for 20 years and it's been heartbreaking to see it decline as it has. It's just the complete lack of resources. There's just no intensive care beds.. ...It's just tragic how the hospital has changed over this time and everybody has been ŌĆ” getting pressure to try and keep the operating theatres closed. I guess it's money. I can't think of any other reason....They shut wards all over the hospital and put offices in there. The hospital has become fuller and fuller of administration management and fewer beds.Obviously they're not getting enough money but they're employing more and more management to decide what they're going to do with the little money they're given, and it's not going through to the patients."
There's the effects of neo-liberalism strategy of starving the public health system of funds. The shortage of beds causes access blockage in the emergency department. Overcrowded ands overstretched emergency departments suggest that some people are turning up at causality departments because they cannot afford or access care provided by GPs.
So governments are crisis managing--putting out spot fires.
Posted by Gary Sauer-Thompson at 12:59 AM | Comments (5) | TrackBack
October 8, 2007
health reform: John Dwyer on
Public opinion polls consistently place health at, or near, the top of any list of public issues important to voters. It has taken them a while, but each of the major parties has broached the topic of health.They have done so in a way that leaves much to be desired since electoral politics overrules health care reform, given the present dysfunctional "system" is constituted by a series of fiefdoms and is characterized by a large number of adverse events.
The real reform need is to reduce the emphasis on hospital care and shift the focus on primary care so as top lessen the number of people going to hospital. That understanding of health policy is not rocket science, is it? Public hospitals have major problems because of ever-increasing demand, under-funding and shortages of health professionals.
John Dwyer, University of NSW professor of medicine and founder of the Australian Health Care Reform Alliance says:
It is madness that states get more money from the commonwealth if they have more overnight admissions to hospitals It costs $750 a day to lie in a hospital bed before you get your first aspirin and much, much more in an intensive care unit or an emergency department. We need better community care. Seventy per cent of the hospital admissions of older Australians who are in very poor condition could be avoided if there was effective community intervention.
We need to swing the healthcare system around to prevention and maintaining wellness and early diagnosis. Half the diabetics in Australia don't know they have diabetes. (Most) people who are going to have a heart attack don't know they have high blood pressure. Countries like New Zealand and Canada have markedly reduced the demand on hospital services by investing in better primary care. It is intolerable in Australia that you are five times more likely to die prematurely from a preventable illness if you live in Sydney's outer west than on the north shore.The continuum of care that should link primary, community and hospital services is made all but impossible because of the inefficiencies associated with the great divide, and the political buck passing, between the Commonwealth and the states.
Posted by Gary Sauer-Thompson at 9:36 AM | Comments (6) | TrackBack
October 2, 2007
the electoral politics of health
The politics of health continue. Health Minister Tony Abbott has foreshadowed a solution to a dogs breakfast health "system". The next five-year commonwealth-state health agreement would require each hospital to have a chief executive accountable to a local board. The measures would follow the model established by the Federal Government when it intervened to prop up the Mersey hospital in northern Tasmania, which will be funded by the Commonwealth but managed locally.

Clements
The justification? Apparently the ALP is engaged in a federal takeover of hospitals so the Coalition is going local. The ALP is actually talking about a single funding for hospitals, not actually running state public hospitals from Canberra.
This shift to placing power in the hands of local communities by the Coalition effectively cuts out the states, and it is at odds with the plans of some States (eg., SA) to do away with local hospital boards as they modernize their health system so that work in terms of a co-ordinated clusters of hospitals, primary care clinics and aged care facilities in a particular region.
It is also ignores the workforce shortages and the lack of resources at the heart of the health systems that necessitates the shift to clusters and co-ordinated and the transformation of some regional hospitals to aged care and rehabilitation facilities.
Update: I October
The crisis in the hospital "system" surfaces most dramatically in the adverse events in cash-strapped public hospitals and with patient complaints. The Age has an editorial on the topic. It says:
Both parties in this hospital war ŌĆö or is it just a phoney war, a blame game being waged by political adversaries with no definite, clearly articulated policies to fix the system? ŌĆö need to focus on issues that get to the heart of the problems in health-care delivery, not tactical manoeuvres that just meddle at the fringes without committing themselves to a real and necessary increase in resources that would go a long way to tackling the system's failures. The Australian public has little interest in the minutiae of hospital funding but knows that more is needed, given that the Government's private health initiatives, and a concomitant decline in realistically indexed federal funding over the past 10 years, have clearly done little to ease pressure on public hospitals. Also, it is more than aware that with growing pressure on hospital beds, the imperative for an early, and sometimes premature, discharge has increased.
The Age's editorial says that rather than pointing the finger at the states and threatening federal takeovers, the Government, or should it win office the Labor Party, needs to deal with the implications of an ageing population ŌĆö for example, by boosting the number of nursing home places, which will free hospital beds for those who are ill, not just old. More beds means more doctors and nurses to attend them, and the next Government must ensure there are enough university places available to train them.
Posted by Gary Sauer-Thompson at 5:33 PM | Comments (31) | TrackBack
September 28, 2007
good governance
Whilst I was at the Australian Psychological Society's annual conference in Brisbane this week, I noticed that Joe Hockey, the federal Minister for Employment, was giving an address athe Brisbane Press Club in the Brisbane Exhibition and Convention Centre where the conference was being held. I didn't attend, and so I don't know what Hockey said but this op-ed in the Sydney Morning Herald can stand in its place.
In it Hockey argues that:
Good governments should be in the business of building opportunity, not imposing its views on others through overt regulation.....And the best foundation upon which to build opportunity - whether it be social, environmental or individual - is a strong economy....Significant government polices do not operate in isolation. Indeed, a government bolstered by a strong economy is better able to implement them. Tackling problems such as the water crisis or climate change is not cheap.

Wilcox
Shouldn't governments be concerned about a healthy population. Providing an opportunity is a means to wellbeing not the end of government policy. Hocky implies that a strong economy is the end of governance, and this can be reinterpreted to meaan prosperity. So Hocky understands wellbeing as prosperity.
Being wealthy equals quality of life, in other words. This view is contested by Lindsay Tanner,the Opposition finance spokesman, who argues that:
time is the currency of relationships. We use money to buy goods and services, but we use time to build and sustain relationships.The pressures of modern life are eating into our time and making it harder to lead a balanced, fulfilling life. Everywhere you look, you will see battles about time at the heart of contemporary political controversies. ...In contemporary politics, relationships are an afterthought. Everything revolves around measures of material wellbeing. The health of our relationships is just as important, but it's harder to measure. So it's usually ignored.
He adds that material wellbeing is at the centre of Labor and Liberal traditions and that it has taken decades for environmental sustainability to come to prominence. It has with climate change.
Posted by Gary Sauer-Thompson at 1:29 PM | Comments (12) | TrackBack
September 23, 2007
adverse events in Victorian hospitals
I have referred to adverse events in Australia's public hospitals before as well as the culture of denial that exists within the medical administration and profession. We have another example from emergency care in Victorian hospitals.
Dr Andrew Buck, of the Monash Medical Centre, alleges that the shamefully chaotic state of Melbourne's hospital emergency departments is jeopardising patient safety, compromising doctors' mental health and leaving health-care agencies exposed to negligence law suits. He is actign as a whistle blower despite a regime of open disclosure being put in place in Victoria.
In a letter to the state's top health officials ŌĆö sent to Health Minister Daniel Andrews and leaked to The Sunday Age ŌĆö Dr Buck, a senior emergency registrar at Southern Health, says despite Monash Medical Centre buckling under record numbers of patients during the recent flu and gastro outbreaks, no extra staff were put on to help manage the crisis. Buck says:
When I came to work on Monday night all cubicles were full and there were 14 'likely admission' patients waiting to be seen and seven 'likely discharge' patients waiting, and some of these had been waiting up to eight hours to be seen.That night, even when an elderly woman suffered a cardiac arrest and died in the emergency department, there were "no extra staff put on to cope with the workload, and there was still no communication from my superiors ŌĆ” about risk management or bypass procedure".It left me with a real sense of hopelessness about any chance for improvement in our working conditions. If this didn't trigger action on behalf of management what would? A death in the waiting room? Multiple deaths? I was appalled that patients' lives are being put at risk, my workload and stress levels, and risk of negligence claims are allowed to escalate unchecked purely so that the hospital can receive a funding bonus.
Dr Buck said that while he could comment only on his experiences of overcrowding and under-resourcing at Southern Health, he was "positive that this situation is being replicated" across town.
According to this Senate Report in 2000 by the Senate Community Affairs Committee there is little data on adverse events in Australia. The Report states that in 1994 the Quality in Australian Health Care Study (QAHCS) was commissioned by the then Commonwealth Department of Human Services and Health to determine the proportion of admissions associated with an adverse event (AE) in Australian hospitals. This was the first published study in Australia that attempted to identify quality of care problems in Australian hospitals and the Senate Report states that:
The QAHCS study found that 16.6 per cent of hospital admissions were associated with an adverse event and 51 per cent of the adverse events were considered preventable....While in 77.1 per cent of cases the disability had resolved within 12 months, in 13.7 per cent the disability was permanent and in 4.9 per cent the patient died. For the two categories of ŌĆśdeathŌĆÖ and ŌĆśgreater than 50 per cent permanent disabilityŌĆÖ, the proportion of high preventability were 70 per cent and 58 per cent respectively.
The Senate Committee considered the extent of adverse events disturbing. The implications in terms of preventable adverse outcomes and the use of health care resources are substantial, especially as the Quality in Australian Health Care study suggests that in up to half of all adverse events practical strategies may be available to prevent them.
Posted by Gary Sauer-Thompson at 1:52 PM | Comments (4) | TrackBack
September 15, 2007
from patient to consumer
In Who Owns our Health? Medical Professionalism, Law and Leadership in the Age of the Market State Thomas Faunce explores the consequences for our medical profession as global health care and pharmaceutical corporations progressively implement a strategy to fully privatise health service delivery and access to medical systems in Australia. He says:
At present universal public health systems based on taxpayer-funded equality of access still have great popular support. The majority of citizens in most developed nations appear to view high tax rates as reasonable if the payback is greater security and peace of mind as they collectively age and exposed to greater risk of illness.Yet despite this widespread popular support, many governments are still producing health polices that lack any any consistent commitment to such public goods.
A major pressure on the doctor-patient relationship is the way that corporate strategists and lobbyists have facilitated the designation of patients as consumers.
'Consumer' in a market state does equate health care with purchasing commodities such as a house, food or soap powder. This market talk misses the way that illness creates vulnerability and ignores the trust that those suffering illness have in doctors to help them become well.
Update
Peter Saunders, director of social policy for the Centre for Independent Studies, attacks the very idea of the welfare state. He says that the original welfare state operated like Robin Hood, taking money from the rich and using it to help the poor.
But the modern welfare state operates more like a giant piggy bank, taking money from ordinary people and then giving it back again. So people today pay high taxes only to get much or all of their money back as government payments and services. He says that:
we are used to a political model which makes the constant assumption that every problem can be solved by more government funding. We have to reverse that thinking. Take an area like health: what if we treated health the way we treat aged care, where we have transformed the pension system through compulsory superannuation? We could get ahead of the game on health by giving people the choice to set up personal medical savings accounts. The amount they put in is deducted from their tax bill and out of that account they fund their health care. But we don't hear about that because politicians reason that if they can give money to people, they can buy patronage. But think about it: you pay tax and the government gives you a lot of that money back in various forms of welfare payments. Why not just tax us less in the first place?
That effectively replaces taxpayer-funded universal health care with the market model where most people manage their own affairs without having to rely heavily on government to provide them with what they need.
Posted by Gary Sauer-Thompson at 10:14 PM | Comments (1) | TrackBack
September 10, 2007
debating health care?
A recent Age poll shows that health is one of the core election issues with many people, who are discontented with how the "system" is run by state and commonwealth governments. Both are to blame for the poor services because the current federal division of funding and service provision responsibilities means that the state and territory governments are responsible for hospital services, whilst the federal government is responsible for funding GPs and aged care services.
How are the commentators interpreting this concern? Is there a health debate forming in the media? Does the ALP own the health issue?
Fiona Armstrong in this op-ed in On Line Opinion points to the concerns about the sustainability of resources in the health sector. She says:
our ageing population puts pressure on a diminishing and ageing workforce. Ballooning costs associated with rising demand, as well as unprecedented use of technology, are placing huge pressure on health care budgets, while workforce shortages are creating unsustainable workloads for those delivering services. Given the quantum of funds involved (about $80 billion annually) and the inescapable pressures on the health budget, it is vital to ensure funding is delivered by the most effective, cost effective, and equitable means.
Armstrong argues that the separation of funding streams between state and commonwealth governments is a big problem and that it needs addressing as part of the reform of the health "system".
The reason given by Armstrong is that the separation of funding streams leads to:
cost-shifting, fragmentation of services, duplication of services and massive investments in administration in an effort to try to co-ordinate it all, much of which could be reduced and quality of care improved if the system was reformed.
The reform favoured by Armstrong involves shifting to the creation of a single fundholder responsible for financing all of the health services provided to a patient. She says that:
The arguments for a single funder are that it would have the effect of reducing much of the administrative inefficiency, making services more cost-effective, and ensuring a seamless transition between all of the services provided to a single individual. (A single funder does not mean a single supplier - services are generally best provided closest to the patient.)
Mentioned as advocates of this view are John Menadue of New Matilda and the Centre for Policy Development; and Jeff Richardson, economist at the Monash Centre of Health Economics and former chair of the recent review into the Tasmanian health system
Presumably, this single fundholder position implies that the commonwealth is the single funder, as explicitly advocated by Andrew Podger, who favours a full Commonwealth takeover of the financial responsibility of the health system. This is not likely to happen in a federal system of governance. Co-operative federalism is more likely politically speaking, and that would mean some sort of pooled funding arrangement. How would this happen? What steps are required to bring about a single funder? What sort of strategy needs to be developed? Who would do that?
My judgement is that funding is a big issue that no one really wants to tackle as it involves federalism. It has to be tackled around the edges.
Posted by Gary Sauer-Thompson at 3:49 PM | Comments (1) | TrackBack
September 4, 2007
ALP shifts health focus to primary care
The ALP has taken another step to shifting the focus of the health system from crisis care in hospitals to primary care and prevention. It indicates that a Rudd Labor government will continue the process of the reform of the health "system" that the Coalition sees no need for.
Rudd states that a Labor government will spend $220 million to establish "GP super clinics" in regional and outer metropolitan regions. Incentive payments are to be offered to encourage doctors and allied health professionals to bring a broad range of health services under one roof. The purpose of these one-stop shops is to provide local communities with enhanced preventive and multidisciplinary care, particularly for patients suffering chronic conditions. The goal is to improve public health outcomes, create a less expensive health system, and take the pressure off public hospitals.
Labor 's argument is that the new super clinics will provide bulk-billed services in underserviced locations with high levels of need, and that this will prevent non-urgent patients clogging up hospital emergency departments.
Jeremy Sammut, a research fellow at the Centre for Independent Studies, that Labor's argument misses the point:
...the problems in public hospitals are not caused by lack of bulk-billing. (New figures show GP bulk-billing rates have increased to just over 78 per cent.) Research conducted for the Australasian College for Emergency Medicine in 2004 found that non-urgent patients do not significantly add to emergency department workloads and are not the cause of hospital overcrowding. The real cause of delayed admission and long waiting times is high occupancy. The unavailability of acute and elective beds is exacerbated by the number of elderly patients who remain in hospital due to the shortage of ''high-care'' places in residential nursing homes.
This is true. Hence the need to develop residential nursing homes. However, that is not an argument against shifting the focus from hospitals to primary care and prevention, so as to slow the numbers of people entering the hospitals. Sammut acknowledges this as he says:
Labor's plan to address the twin challenges of population ageing and rising incidence of lifestyle disease is to reorientate the health system away from high-cost curative care in hospital towards lower cost primary care in the community. Once diagnosed with a chronic condition such as diabetes, chances are that some patients will work with their doctors to manage their illness and avoid the real risk of acute episodes.
He agrees that good management may well prevent expensive secondary medical interventions, but asks 'do we really need super clinics to provide the stock standard medical care that is delivered every day in doctors' surgeries throughout Australia?' This misses the medical workforce shortage issue and the need to use non-medical health professionals to deliver health care services.
This leaves us with the primary care argument. Sammut's response is a sceptical one:
Advocates of preventive medicine also talk of education as the key to prevention. Of course, health professionals can give commonsense advice about good diet and regular exercise. But I doubt that many people in high- risk categories will modify their lifestyles while the risk of harm remains relatively remote. Investing in primary care to keep people out of hospital sounds like a good idea. But spending more taxpayers' money on preventive medicine is unlikely to prevent lifestyle disease as promised.
Sammut doesn't seem to like the idea of spending money on public health. Is this because CIS is opposed to the public health care funded out of taxation.
Posted by Gary Sauer-Thompson at 6:50 AM | Comments (1) | TrackBack
August 30, 2007
Health reform: first steps?
How far is the political system willing to push for reform of the health care "system", now that the problems of the current are coming to the surface, eg., adverse events and saving hospitals from closure or downgrading due to the lack of qualified staff. How is the health "system" to be reformed to meet the health needs of the ageing population? What instruments will be used to govern reform? Which political party--Liberal or Labor--shows more commitment to the reform process?
An insight can be gleaned from this recent op-ed by Leslie Russell in the Canberra Times Russell, a research fellow at the Menzies Centre for Health Policy says that the origin of the problems currently facing all public hospitals is the way in which public hospitals are funded:
by joint contributions from the Commonwealth and the states and territories through five-year Australian Health Care Agreements, and the lack of any incentives in these agreements for innovation to improve patient outcomes. When the last agreements were signed in 2003, the Commonwealth ignored calls for reforms around better integration of the primary, acute and aged-care sectors, information technology and e-health, quality, safety and workforce, and a push for better indexation of funding. The states and territories received almost $1 billion less under the 2003-08 agreements than expected, and the Commonwealth contribution to the costs of operating public hospitals has fallen so that is now about 40 per cent. The agreements have only one performance indicator on which funding is contingent [on] a commitment to provide public hospital inpatient services at an agreed level.
Russell, a former Labor health adviser to Julia Gillard, comments that at a time when the focus in health is turning to prevention, screening and better management of chronic illnesses, the Commonwealth's approach is a short-sighted one , as it rewards the provision of isolated episodes of treatment for illness rather than efforts to ensure ongoing health.
One can only agree with this interpretation. The five-year Australian Health Care Agreements between the Commonwealth and the States, which is due to be resigned, is not being used as a lever to reform the health care "system" in spite of CoAG's commitment to health care reform. Russell then pinpoints the exact failure:
The agreements fail to recognise that, increasingly, health services are delivered in day surgeries, outpatient clinics and patients' homes. They do nothing to provide resources to ensure that patients can access affordable GP services rather than attend busy emergency departments, and that there are residential aged-care beds for frail elderly patients so they are not left inappropriately in expensive hospital beds.
So which political party is in willing to tackle health reform? Russell argues that it is Labor. She says that its policy
begins the process of moving the funding relationship under the Health Care Agreements towards a greater focus on patient outcomes by offering financial incentives to the states and territories to implement programs to reduce avoidable hospitalisations and readmissions, reduce non-urgent emergency department presentations, tackle waiting times for elective surgery, and help get the frail elderly out of hospital into residential aged care.
What Russell shows is that we have the first steps being taken to a reform pathway. It is not one that begins to engage with the need to deal adverse events and the closure of professional ranks, the failure to keep the public informed of adverse events, the regulation of health professionals, a greater autonomous role of allied health professionals, or the challenge to medical hegemony in funding.
Posted by Gary Sauer-Thompson at 7:16 AM | TrackBack
August 28, 2007
Health system + adverse events
Peter Martin in an op- ed in the Canberra Times refers to the adverse events in our hospitals, and the 1995 ŌĆśQuality in Australian Health CareŌĆÖ study:
Each year some 18,000 of us die in hospitals. By comparison, fewer than 2000 Australians die on the roads. The 18,000 deaths, six out of 10 of which were avoidable, were identified, along with 50,000 cases of permanent disability, in a landmark 1995 study that has never been repeated.
And yet we rarely hear about this. Unlike road deaths they are not publicly reported. Politicians confidently repeat that we have a good health system, whilst the media challenges this by focusing on waiting lists and hospital queues:

Neil
Martin goes on to say that ten years later in 2005, an editorial in the Medical Journal of Australia asked whether a decade on we could "confidently state that health care is safer for patients"?
It concluded:
Unfortunately, the answer is no. It is regrettable that we have not measured the frequency of adverse events in Australia in a way that allows us to assess how we have fared since 1995; how we compare with other countries; and whether any initiatives have been effective in reducing patient harm.
It is not deemed important enough to keep these kind of figures on a national level. What we have is a fundamental failure of governance by both the State and the Commonwealth governments--separately and together --- and the lack of willingness to respond appropriately at both the bureaucratic and political levels. A curtain is being pulled over adverse events.
Professor Jeff Richardson, the foundation director of the Monash Centre for Health Economics, says that an estimated 50 Australians die in hospitals every day. Another 140 are permanently injured. Richardson describes the reported rate of preventable deaths in hospitals as "equivalent to a Bali bombing every three days". He adds that we are probably justified in thinking about those deaths in the same way as we would a casualty rate in a war.
Posted by Gary Sauer-Thompson at 7:09 PM | Comments (8) | TrackBack
August 23, 2007
Michael E. Porter on health care reform
I've been digging around the internet looking for pathways --information flows--- that would take me outside the current horizons of the Australian media, magazines and bloggers. I'm finding it a bit insular, the quality of the contents of the op-ed columns in the mainstream media is dropping, the online subscription based media are not breaking new ground and there is not much interaction between political bloggers and journalists.
I've come across something that is connected to my interest in health care--- an independent group-blog on health care called World Health Care Blog. Independent here means that there a number of health bloggers run their own blogs but contribute to a group health blog set up under the Corante umbrella.
It is US in orientation, and all the bloggers reside in the US, which undercuts the blogs claims about being a world blog.There is a link to a 4th Annual World Health Care Congress, which once again is about the USA. The session on competition in health care led by Michael E. Porter, at The Institute for Strategy and Competitiveness is interesting. On the video Porter highlights the need to restructure the delivery of health care to increase value.
This is more than cost containment (a dead end) and reducing administrative costs, as the vast majority of cost are in the actual delivery of care. The restructuring needs to be major on not an incremental one.
This is because the management and organization is a 19th century one whilst the medical technology is 21st century. The best approach to getting improved value is to move the organization from medical specialties to medical conditions, a cycle of care and integrated practice units.
Yet competition has not delivered on improving value in health care delivery. Why so? Porter argues that what we have is bad competition in health care, as it is concerned with zero sum competition (cost shifting, capturing more revenue and restricting services etc) and not with the health outcomes for consumers. The fundamental flaw in the health care sector is not competition, but the wrong kind of competition. Healthy competition is competition to improve value for customers.
Porter's talk is based on his book Redefining Health Care This text clearly recognizes that the U.S. health care system is on a dangerous path, with a toxic combination of high costs, uneven quality, frequent errors, and limited access to care. The many disparate kinds of evidence, taken together, lead to the same overwhelming conclusion: the system is broken, and the magnitude of the problem is staggering.
it is is similar situation in Australia. The health "system" is on collision course with demographic and economic reality. Reform efforts have failed because the diagnosis of the problem was wrong and the attempts to treat the system have addressed the wrong issues or offered piecemeal, ultimately ineffective solutions aimed at symptoms rather than causes.
Posted by Gary Sauer-Thompson at 1:58 PM | Comments (3) | TrackBack
August 9, 2007
health governance, Howard style
Jeff Richardson, a health economist and Foundation Director of the Centre for Health Economics at Monash University, is critical of the Howard Government's $45 million intervention in Tasmania to "save" the Mersey Hospital. As we know the Lennon State Government, after a second review of services had announced in May that the Mersey would not close. It would lose its intensive care and many specialist surgery units and be downgraded to an elective day surgery and rehabilitation centre. Richardson comments:
The state plans were to add aged services, renal dialysis, rehabilitation, a 24-hour emergency centre and high-speed ambulance services to nearby Burnie. Many small population areas in Australia have a far inferior service...Howard's intervention will cement in place a system in which adverse events will flourish and in which Tasmanians will die unnecessarily. First-class specialists seek to practise in centres of excellence and it is hard for Tasmania to achieve these even in Hobart and Launceston.
In 2004, he undertook a detailed study of the Tasmanian health system in which he recommended a scaling back of complex procedures in smaller country hospitals because they couldn't get the specialists with the necessary skills and experience to perform such procedures safely. Even if they could, the population of north-west Tasmania is too small to generate the clinical workload to keep their skills honed to world standards.
The study recommended that one large, not two small hospitals in North West Tasmania should provide comprehensive specialist services. This would allow the delivery of safe world class, not second class, specialist services.
It's not just a case of skilled staff being flown in from time to time. We also have the problem of adverse events--- mistakes which would not have occurred in a higher quality system. Richardson refers to a study in 1995 on quality of health care in the Medical Journal of Australia that estimated that at least 10 per cent of hospital admissions are associated with an adverse event including up to 9000 unnecessary deaths annually. He points out that:
these events are not primarily the fault of doctors (who make mistakes like all of us) but of systems which have not been properly designed to avoid errors and which force doctors to work in unsafe hospitals.
So there is a danger that adverse events would continue in a "saved" Mersey hospital. Richardson says that for political reasons, it is unlikely that Burnie specialist services will be trashed. It is more likely that two hospitals will be allowed to struggle for existence, providing second class medical care as in the past ŌĆö thus ensuring the continuation of adverse events.
Posted by Gary Sauer-Thompson at 2:24 PM | Comments (5) | TrackBack
July 29, 2007
AMA: money talks
This is the speech given by AMA President, Dr Rosanna Capolingua, to the National Press Club, last week. I was interested in it as I had visited the GP last week and experienced a bad time.Though the GP was a referral mechanism my need for yearly checks ups for skin and prostrate cancer was questioned. I was sucking their Medicare dry.
I fought the GP who had not read my file for the followup referrals, and it cost me over $50. This was charged to my credit card and I would need to wait for several weeks for the refund to be posted. The GP was being paid to be the gatekeeper to the health system. There was little to no interest in preventative care.
I was also interested to read what the AMA considers the health issues to be in the federal election, as little--nothing---is being said about health by either side. A number of issues are canvassed by Capolingua in the speech: Indigenous Health, overseas trained doctors, public hospitals, aged care, rural health, national registration, Medicare easy claim and it is acknowledged that health health policy is the ŌĆśsleeperŌĆÖ in this election.
So things looked promising.
I was curious about Medicare Easypay It sounded good as the idea is that the patient will be able to get their Medicare rebate at the point of service when they pay the practice account. Just like the private health funds do when I see the chiropractor for preventative care.So where does the AMA stand?
Opposed, even though Capolingua starts the speech by saying that for the AMA patient care is the primary driver always has as its primary driver and in the forefront of doctors minds. Here's the relevant bit of the speech:
Patients will have to wait while the doctorsŌĆÖ receptionists need to spend more time processing each patient. I can see mums with one sick kid on the hip and a toddler running away, trying to pull out three cards ŌĆō credit card, Medicare card and debit card - at the front counter to have the account processed. if it takes only one extra minute per patient, this could be an extra three hours work per day in a busy four-doctor practice. So far, some practices have got it down to four minutes a patient! That makes 12 hours a day! There will be additional keying in, and processing failures of up to 20 per cent as now occurs, and the system will take a long, long time and more staff and more EFTPOS terminals to reach efficiency. Remember the Medicare queue? I do not want my patients to suffer that in my surgery.
What? That reads as if the AMA want to be paid by Medicare to process the transactions far more than a concern for patient care.
This interpretation is supported by Jason Koutsoukis who was present at the speech in the National Press Club. He says:
It took a while, but eventually Capolingua let the cat out of the bag.The real reason the AMA doesn't like Easyclaim is because they want some extra cash in their pockets every time they process a payment ŌĆö about $1 per transaction which, if you add up how many patients the average GP sees each year, could turn into quite a nice little earner funded by taxpayers. It turns out that pharmacists get a 40-cent transaction fee every time they process a pharmaceutical benefits scheme claim and the doctors want to be compensated, too.
So there you have it. Medical politics. It's about power not patient care.
Posted by Gary Sauer-Thompson at 6:37 PM | Comments (2) | TrackBack
July 6, 2007
Blogging the Adelaide Festival of Ideas 2007
I walked into the 2007 Adelaide Festival of Ideas for the mid morning session in the delightful Bonython Hall on food entitled Before You Eat. It was hosted by Norman Swan, who runs the Health Report on your ABC. The session was introduced by Swan as a conversation amongst the participants on the politics of food. with the audience able to ask questions at any point. The session rambled over many topics as conversations do.
Marion Nestle kicked it off by introducing the industrial system of food or agri business that externalizes the cost of production (polluted rivers), has huge waste problems and produces poor quality food The reaction to this in the form of the sustainable family farm or organic farming. So we are faced with choices about the food we eat.
Kerin O'Dea argued that if change what we eat then we have to change the food supply. Instead of sending market signals to farmers to produce lean met we pay by the weight and so we have fatty meat. The food supply is not connected to public health.
Peter Clifton deepened this insight by arguing that as water is the crucial issue for Australians so there needs to be a trade of between the water used and the calories produced. So we weigh up white rice and an animal source of protein that also contains vitamins and minerals as a balancing act.
Clifton argued that as food production is efficient in Australia, food is cheap, Australians eat too much and so they become obese. I would have thought that junk food makes us fat and that there is a class divide around food: the middle class eat good quality food whilst the working class eats fatty food. That's what promotes obesity. The politics of food is a class issue. Even though we are surrounded, seduced and tempted by junk food, eating good food does matter in terms of our health or wellbeing.
A number of interesting questions were raised by audience about antibiotics in industrial produced chickens, the effects of gene technology on farmers, the greater inequality in diets, what our diets would be in 2040 given the effects of climate change---shortage of water and increased cost of energy.
Posted by Gary Sauer-Thompson at 7:41 PM | Comments (3) | TrackBack
July 5, 2007
Adelaide Festival of Ideas 2007: eat well be well
 Suprisingly, given the low profile of health issues in the federal election, the 2007 Adelaide Festival of Ideas has a strong theme of health running the different sessions with a strong emphasis on good nutrition. Eat well be well is an argument running through the 'Before You Eat' session on Friday. Kerryn Goldsworthy at Pavlov's Cat has some interesting comments on this.
Suprisingly, given the low profile of health issues in the federal election, the 2007 Adelaide Festival of Ideas has a strong theme of health running the different sessions with a strong emphasis on good nutrition. Eat well be well is an argument running through the 'Before You Eat' session on Friday. Kerryn Goldsworthy at Pavlov's Cat has some interesting comments on this.
It is most explicit in Marion Nestle's ' 'What to Eat' talk on Saturday which takes us into food and health policy. Fox News, that Republican cheer squad, is not impressed by this kind of approach, which it sees as another example of junk science.
This approach works within the health policy reform agenda of prevention and primary care. This health reform argument persuasively expressed by the Centre of Policy Development is a simple one:
Governments are always talking about taking the pressure off public hospitals and reducing spiraling costs. The current Howard Government says it can do it by subsidising the Private Health Insurance industry, which hasn't worked. The states argue that they could cut hospital waiting lists if only the feds gave them more money. Both arguments miss the point. The best way to take the pressure off hospitals is to ensure that most people don't need to go there in the first place.
Australia faces spiraling rates of chronic illness, including many that could be prevented, mitigated or cured through early intervention. Without change, we will keep spending more and more to achieve less and less. Too many people have to fight their way through a complex maze of services and funding systems to deal with common illnesses that could easily be addressed at their local health centre or family medical and non-medical practice.
What is missing is the willingness of state and federal governments to take on the challenge of real health reform despite obesity being a real problem. The establishment of 'one stop shop' primary health care centres staffed with all the expertise needed to manage the overall health of the local population. These centres would form the backbone of a high-quality universal health system, benefiting Australians of all backgrounds and incomes, rather than a limited ŌĆśsafety netŌĆÖ service designed to catch the fallout from a two-tier system.
Robert Phiddian's notes for the 'Before You Eat' session say that though food is at the centre of our lives constantly, a social as well as a physical staple, we in the developed world are further from the production of food than we have ever been before. The chain from farm to plate is now fantastically long and increasingly invisible to individual consumers, many of whom even do precious little cooking these days.
He says that his main point is that the food chain is attenuated, and we consumers donŌĆÖt know much about what we are putting in our mouths. In particular, we could afford to know more about any or all of:
the risks to health (real as opposed to imagined) from chemical inputs in the food chain; the costs and benefits to individual health of highly processed foods; the costs (nutritional as well as environmental) of having everything in season all the time; the further dietary implications of affluence that mean most people in the developed world can eat what would once have been luxury foodstuffs most of the time; the alleged ŌĆśobesity epidemicŌĆÖ and what we can do about it.
We are right in the core of food and health policy. Nestle's talk, based on her 'What to Eat' book, directly tackles junk food and food politics from a health perspective. As she observes when it comes to the mass production and consumption of food, strategic decisions are driven by economicsŌĆönot science, not ethics, and certainly not health.
A consumer driven society we have lost sight of wellbeing as a flourishing life understood as healthy functioning. We are reaping the consequences with obesity and ill health.
Posted by Gary Sauer-Thompson at 12:15 PM | Comments (4) | TrackBack
July 1, 2007
Weekend question: about healthcare
Why is health on the backburner in this federal election. Is it because Australian's have a really good healthcare system? Is it because of bipartisan consensus on health? Is it because Tony Abbott has effectively neutralized health as a political issue? Is it because the ALP has little to say because it has run out of ideas after Medicare Gold was relegated to the historical bin? Is the concern about a two tiered health system lessening?
There is a consensus that the federal government should provide support to all Australians through Medicare and the pharmaceutical benefits scheme; that taxpayers should subsidize private health insurance and that the management of public hospitals should be left to the states.
Health has fallen off the political agenda, even as prevention becomes the new buzz word in health policy. Little is said about doctors being wined and dined by drug companies under "educational" events, and the way GP's are corrupted by these practices.
Does the ALP have a health policy? Not really. Medicare Gold has been pushed to one side. There have been vague commitments about improving relations with the states, reintroducing the commonwealth dental scheme and addressing the prevention of chronic illness. Labor has lost its leader in the Australian health policy debate by default.
Last week Opposition Leader Kevin Rudd did release Labor's health policy entitled "Fresh ideas and future economy", it focused on preventive health care. Rudd Labor is aware that the cost of providing health care and the cost of rising demand for health care is expected to spiral--- the commonwealth Government spending on health care will increase from 3.8 per cent of GDP in 2006-07 to 7.3 per cent in 2046-47 and that poor health adversely affects work performance and productivity.
Rudd Labor argues that the best way to equip our health system to deal with the challenges of the future is to end the blame game and re-invigorate the role of the primary care system ŌĆō the front line of the health system which provides health care to local communities. So it will:
Develop a National Preventative Health Strategy to provide a blueprint for tackling the burden of chronic disease currently caused by obesity, tobacco, and excessive consumption of alcohol. The Strategy will be supported by an expert Taskforce.
Shift the focus from so-called ŌĆ£six minute medicineŌĆØ in general practice by beginning a reform process to provide incentives for GPs to practice quality preventative health care;
Broaden the focus of the major health care agreement between the Commonwealth and the States and Territories beyond hospital funding by developing a National Preventative Health Care Partnership; and
In its first term, commission the Treasury to produce a series of definitive reports on the impact of chronic disease on the Australian economy, and the economic benefits of a greater focus on prevention in health care.
This sounds good but there is not enough detail to pass judgement.
Posted by Gary Sauer-Thompson at 5:40 PM | Comments (8) | TrackBack
June 15, 2007
Medicine's Working Group + PBS
One of the research projects of Thomas Faunce, a senior lecturer in the medical school and the college of law at the Australian National University, is investigating the impact of international trade agreements on Australia's medicines policy.
In a recent op-ed in The Age he argues that the Medicines Working Group, established under the free trade agreement between Australia and the United States, has played a significant role in creating the controversial changes to reference pricing arrangements for patented medicines under the Pharmaceutical Benefits Scheme, now in legislation before the Senate.
Faunce asks whether the agenda of the Medicines Working Group is similar to that of the US negotiators to the trade agreement, who had been required by legislation to seek the "elimination" of reference pricing under the PBS. He says that:
Australia's approach, expressed clearly in Annex 2C of the free trade agreement, was to value pharmaceutical innovation scientifically through expert assessment of its "objectively demonstrated therapeutic significance". This is the task of the existing Pharmaceutical Benefits Advisory Committee. It is a crucial part of such transparent, evidence-based assessment that new patented products be assessed for innovation against all available therapies, generic or even non-medical, for the same main clinical indication. If a new drug can't prove that it works better and is safer for a reasonable price difference than an existing generic competitor, why should the community have to pay more over time for its technical molecular flamboyance or associated advertising?
He says that the position of the the US medicines negotiators to Annex 2C (on pharmaceuticals) of the agreement was that new patented medicines should not have their claims to "innovation" assessed by comparison against cheap generic medicines.
This is crucial as one of the key drivers of rising health costs over the next decade is the PBS. The agenda of the Medicines Working Group would increase Australia's health care costs. We know that the text of the Agreement increase the pricing power of US drug companies operating in Australia. So it is unlikely, based on past practice, that they will not make use of that new pricing power.
Most of the measures in the FTA apply to new drugs rather than existing ones. In a submission to the Senate on the FTA and the PBS Faunce, Drahos and Henry argue that it is:
plausible that the gap between US and Australian drug prices could be cut in half. We estimate, very conservatively, that AustraliaŌĆÖs PBS will have to pay at least one third more for its drugs with the FTA than without it. If the likely FTA effects are applied to 2003 figures, the extra cost to of the PBS to the government last year would have been around $1.5 billion for the same drugs at the same levels of use and with no increase in the health benefit to Australian patients. Similar pressures would be felt by other buyers of prescription pharmaceuticals, particularly hospitals.
Drug prices are around three to ten times lower than in the US because of this reference pricing policy. Will there be a new category of medicines (known as F1), which will not be subject to reference pricing, and for which the government will pay much higher prices?
What does that mean for co-payments? Isn't the commonwealth government seeking savings of $580 million over four years due to lower wholesale prices paid by the government for generic versions of some common medicines with expired patents? Will the higher prices be passed onto consumers?
He asks whether the agenda of the Medicines Working Group is similar to that of the US negotiators to the trade agreement, who had been required by legislation to seek the "elimination" of reference pricing under the PBS. He says that:
Australia's approach, expressed clearly in Annex 2C of the free trade agreement, was to value pharmaceutical innovation scientifically through expert assessment of its "objectively demonstrated therapeutic significance". This is the task of the existing Pharmaceutical Benefits Advisory Committee. It is a crucial part of such transparent, evidence-based assessment that new patented products be assessed for innovation against all available therapies, generic or even non-medical, for the same main clinical indication. If a new drug can't prove that it works better and is safer for a reasonable price difference than an existing generic competitor, why should the community have to pay more over time for its technical molecular flamboyance or associated advertising?
He says that the position of the the US medicines negotiators to Annex 2C (on pharmaceuticals) of the agreement was that new patented medicines should not have their claims to "innovation" assessed by comparison against cheap generic medicines.
Posted by Gary Sauer-Thompson at 12:32 AM | Comments (2) | TrackBack
June 1, 2007
medicine's woes
Is medicine facing an era of perplexing stagnation? It would appear to be so. Consider the remarks below by Richard Horton in the New York Review of Books, made whilst reviewing James Le Fanu's The Rise and Fall of Modern Medicine: The argument of the book is that despite the significant advances in combatting disease which reached their peak in the post-war years, the promise of modern medicine at the end of the century has failed to materialise. Horton says:
Doctors are disillusioned by their profession; they increasingly have to deal with "the worried well" rather than the genuinely sick; they have to contend with the puzzling and, for many physicians, irritating popularity of alternative medicine; and the costs of diagnosis and treatment are escalating at a rate that is not matched by advances in knowledge. From the 1970s onward, there has been "a marked decline" in innovation. And, worst of all, doctors have experienced a "subversion, by authoritarian managers and litigious patients, of the authority and dignity of the profession.
The medical profession has problems and is in trouble. Le Fanu's account is one of the fall of medicine. After the golden age---when medical science has reached its natural limit---medicine has suffered from the retreat from rationality that marked the latter part of the twentieth century.
Le Fanu, who longs for the past authority enjoyed by doctors and for the deference that such authority demanded from patients, argues that the intellectual vacuum of the late 1970s was filled by two different sets of ideas, which emerged from two specialities which up until then had played only a marginal role in postwar medicine: genetics and epidemiology (the study of the patterns of disease). The developments in "the new (molecular) genetics," opened up the possibility of identifying the contribution of defective genes to disease. The epidemiologists insisted that most common diseases, such as cancer, strokes and heart disease, were due to social habits-an unhealthy lifestyle or exposure to environmental pollutants. Le Fanu says:
the great promise of the new genetics or of the social theory of disease has not held up according to the author. The amazing strides in our knowledge derived from molecular biology led to the rapid acceptance of the possibilities of gene therapy but these have emphatically failed to deliver, despite the intellectual satisfaction that these smart ideas generate. Similarly, in the wake of studies showing a clear epidemiological correlation between smoking and lung cancer the social theory has sought to link almost every disease for which there is not an obvious infectious cause to some lifestyle or nutritional source mostly blamed on Western society.
Le Fanu's opposition to the social theory of disease---how you live influences how you die-- is greater than his skepticism of genetics.
Their failure explains "the fall" of modern medicine and the source of its present discontents associated with unhappy doctors and the worried well. Raymond Tallis in Hippocratic Oaths: Medicine and Its Discontents gives expression to the former.The crisis in medicine is not a crisis in the practice of medicine or within the system of our health care. The crisis lies within the profession and is due to the acute loss in status that doctors have felt in recent years. Medicine is in danger of becoming "the first blue-collar profession". Doctors are now little more than tradesmen. Tallis sees medicine through doctors' eyes--not the eyes of autonomous patients'.
Posted by Gary Sauer-Thompson at 2:41 PM | TrackBack
May 24, 2007
health care: ALP slips up
Mike Steketee's op-ed, ' Evidence of illness not a private matter', in The Australian is important as it addresses the politics of health, which is rarely mentioned these days as a hot button issue. He says that Health Minister Tony Abbott's favourite way of taunting Labor is to say the Howard Government is "the best friend Medicare has ever had".
This is actually chanted in Parliament by the Coalition MP's during Question Time at the end of Abbott's reply to a dorothy dixer. Abbott leads the chant. The ALP rarely asks questions on health these days, let alone searching ones. Abbott has done his job well--negated the ALP's ownership of health.
Steketee says that this kind of taunting by Abbott:
.. hurts because Medicare was the Hawke government's proudest social policy initiative, but the Coalition has had great success appropriating it for its own purposes. In 1993, when Paul Keating had an unexpected election win not only by campaigning against the GST but also against the Coalition's anti-Medicare stance, voters preferred Labor over the Coalition on health policy by a margin of almost 25 per cent, according to the Australian Election Survey, a detailed opinion poll conducted by academics after each election. By 2001, this gap had narrowed to 13 per cent and in the 2004 election it shrank further to 6 per cent.
Abbott rubbed the sore hard last week by saying that Kevin Rudd had not even mentioned health in his budget reply speech, and he then trumpeted the Government's budget measures.
Steketee is dead right on this. Abbott runs circles around the ALP on health. And the ALP allows him to. They just sit there and squirm. Federal Labor realize that they've dropped the ball, that Abbott has it, and that they are not doing much to get he ball back. Maybe they are hoping that it will slip from Abbott's hands?
The ALP has let this issue slip even though the Government has used the cover of Medicare to engineer a large shift of health resources from the public to the private sector. The shift to private health has induced higher health costs since doctors are able to charge more for private patients, and private health funds are less able to control costs than a single national insurer. Yet the ALP has let the issue slide to the backburner.
Steketee says that Labor has been holding its fire on health announcements but it has no appetite for picking a fight with the private sector. In terms of healthcare reform, it cannot go back to the fully fledged welfare state and it must live with the mixture of public and private health when it addresses the rising costs of health care as well as as quality, access, efficiency and equity.
Posted by Gary Sauer-Thompson at 9:24 AM | Comments (19) | TrackBack
May 8, 2007
heath: cost containment of PBS?
Dr Lesley Russell, a former health policy adviser to the ALP, has an op-ed in the The Age about the forthcoming legislative package introduced into Parliament by Tony Abbott, the commonwealth Health Minister This legislation will implement changes to the Pharmaceutical Benefits Scheme (PBS) scheme that build on the 12.5 per cent generic price reduction policy introduced in August 2005. Behind this sits the Intergenerational Report and the need to contain health care costs, especially the projected growth in the expenditure of the PBS.
The op-ed gives an insight into neo-liberal mode of health governance. Russell says that:
That policy has proved a bonanza for the Treasury coffers, but costly for consumers. The mid-year economic and fiscal outlook showed that for the first half of this financial year, PBS savings were $270 million more than expected and more than covered the $225 million spent on newly listed medicines. But patients' out-of-pocket costs for their essential medicines continue to rise due to premiums added by manufacturers and fees added by pharmacists that do not count towards the PBS safety net, the threshold for which has also increased.There is nothing in this new legislation that will guarantee that consumers will pay less for their PBS prescriptions, and there is every reason to believe that they will pay more.
She says that a major flaw in the Government's package is that it does nothing to build and support a domestic generic pharmaceutical industry so that it can provide real competition leading to the sort of price reductions the introduction of generics brings in other developed countries.
Russell adds that:
In the guise of protecting the sustainability of the PBS, the Government has increased co-payments by 21 per cent, increased the safety net thresholds, and allowed brand premiums and special patient contributions to be applied to one in six medicines listed with no attempt to measure the impact on the health-care system and on health outcomes in the population. The huge savings are not reinvested in health care, despite the growing need for programs to tackle prevention and better management of chronic illness.
What we have with the Howard Government is a focus on costs and budgets rather than health outcomes. Government is seen as a corporate entity with an obsession about debt and finance. So the neo-liberal strategy is for costs to be moved off budget through user pays and onto the community. Through cost shifting the community comes to bear an ever greater part of the growth in outlays.
Posted by Gary Sauer-Thompson at 10:43 AM | Comments (2) | TrackBack
May 4, 2007
bureaucrats redesigning the health workforce?
I attended the national Health Workforce forum in Melbourne yesterday. The forum is designed to help implement the National Health Workforce Strategic Framework, which addresses health workforce shortages and maldistribution against a background of demographic change, new technologies and empowered consumers.
This policy reform is concerned less with the continuation of the status quo with ever larger numbers of doctors and health care professionals and workers,which seems to be the position of many state premiers, and more about future changes in the kind of health workforce in Australia. For instance, the Health Workforce Strategic Framework recognizes that the more difficult issue will be that:
the types of healthcare workers may change and that these changes will be deeply impacted by technology. So ensuring the right practitioner mix will be crucially important and this is likely to involve a mixture of new disciplines and new roles for old disciplines. Boundaries and established professional roles will need to evolve; and new knowledge and skills be acquired, maintained and expanded. In turn, all this will place a greater focus on the length of education and training and the content of education and training programs.
So what we have is decade-long state planning in a neo-liberal world. The mixture of planning and market forces undermines the conventional view that the struggle against socialist planning in a social democratic Australia is over.
Friedrich Hayek or Milton Friedman, of course, would have regarded this kind of planning as presupposing the elitist belief that naive rationalist bureaucrats can be trusted to advance the public good and denounced this planning as socialism by the centralized state as interference of the state in the life of the individual. If cutting taxes is often advocated as a way of constraining the centralized, planning state, then the critique would be directed at the knowledge presupposed by the planners.
Contemporary neo-liberals would, no doubt, follow Hayek in firing their well directed arrows at the fatal conceit of the bureaucrats--their undue faith in the power of a 'constructivist rationalism' to subject society to control through planning, and so ignores the fact that civil society is a "spontaneous order".
However, the current situation more complicated than that, since the rational bureaucrats know that the impetus or driver of major reforms to make the health system more responsive to patient needs, and more focused on preventative primary care , will come from consumer pressure----ie., Friedman's consumer sovereignty. Consumer pressure will motivate the reform-fatigued politicians to continue with ongoing reform of the health care system.
Of course, the neo-liberal heirs of Hayek and Friedman interpret consumer sovereignty in terms of the egoistic drives of possessive individuals pursuing their desires and so focused on finding happiness in financial wealth and consumption. However, the health consumers are not short-term utility maximizers of neo-classical economics as they are concerned about health, and preventing themselves from becoming sick and and wellbeing. What we have is a new politics of well being.
In Australia the politics of wellbeing, that is based on policies of time and care, is argued for by Clive Hamilton at the Australia Institute, and the way it understands wellbeing can be seen from The Wellbeing Manifesto.
However, it is true that in a neo-liberal mode of governing health financing is the major driving force behind reforms. Whereas equity was the dominant issue of earlier decades, the 1990s saw it displaced by the issue of financing and expenditure. Tjis is more than cost containment, as there are changes in the underlying principles of the health system, since health care becomes a 'commodity' and care recipients 'consumers'. Greater emphasis is placed on goals such as increased outputs for decreased inputs, performance and efficacy, quality assurance and financial accountability, and evidence-based evaluation.
Posted by Gary Sauer-Thompson at 12:37 PM | Comments (2) | TrackBack
March 28, 2007
health reform, professional self-regulation, Tony Abbott
In his ŌĆśHealth Reform: Important but easy to overrate speech to the Australian Financial Review Conference at the Sydney Marriott Hotel on February 2007 Tony Abbott, the Minister of Health and Ageing, strikes a warning note about reforming Australia's health care system. He says that:
The ŌĆ£health reformŌĆØ debate has three recurring themes: changing the way public hospitals are managed; ŌĆ£big bangŌĆØ restructuring to end the blame game between Commonwealth and state governments; and renegotiating the Health Care Agreements in ways which keep the structure but change the outcomes.
This account overlooks the structuring themes around health workforce issues and the regulation of the health professions.
Regulation of health professions(medical and non-medical) is a health reform in the light of the failures of professional self-regulation to ensure public safety, most notably with the case of Dr.Jayant Paytel in Queensland. CoAG has moved in this direction with its proposal for a national registration and accreditation scheme under the National Reform Agenda. This scheme proposes a single regulatory body to ensure public accountability.
This shift to national registration is part of the CoAG's response to the Productivity Commission's important Report on Australia's health workforce.
Minister Abbott's reluctance for reform can be seen in his responses to CoAG's national registration and accreditation scheme in his speech to Global Access Partners Conference, Parliament House, Melbourne on 16 February. He states:
The draft scheme circulated last year proposed a single national health registration board with authority over all the professions. A national advisory committee (perhaps comprising the chairmen of the various national registration boards) now seems more feasible. This committee would meet regularly to discuss issues of common interest and would report to the Health Ministers' Council but would not have authority over the professions' individual national boards. It would operate in much the same way as the committee of medical college presidents, a sounding board for ideas and a forum for finding common ground.
This rejection of a single regulatory body that would ensure the accountability of professional self-regulation is a rejected by the Minister in favour of the continuance of self-regulation. Minister Abbott adds:
Some of the professions are concerned that any national health registration board could be used to determine function rather than competence. As far as the Commonwealth is concerned, national health registration is about guaranteeing public safety, enabling portability of practice and reducing red tape. It's not about changing existing professional demarcations.
That leaves the professions investigating and adjudicating public complaints against bad practice with little by way of public accountability, even though the history of self-regulation shows the health professions frequently closing ranks against the public so as to protect their own.
The Minister, it would seem, has been captured by the AMA, which is resolutely opposed to any regulation of its autonomy or self-regulation by a single regulatory body
Posted by Gary Sauer-Thompson at 10:58 AM | Comments (2) | TrackBack
February 21, 2007
doctors and self-regulation
I see that doctors in the UK may well lose their right to self-regulate (vet or police themselves) under a shake-up of their professional regulation. The General Medical Council (GMC) is likely to lose its powers of adjudication in fitness-to-practise cases and its professional elected medical majority could disappear. These responses are part of a set of reforms aimed at preventing another Harold Shipman tragedy, the medical scandal at the U.K.'s Bristol Royal Infirmary, and the ongoing professional cover ups and closed ranks. We are dealing with a history of the medical profession that is littered with mal practice and professional mis-conduct.
As Sir Liam Donaldson, the chief medical officer, says in Good doctors, safer patients times are changing:
...medical regulation has traditionally been synonymous with ŌĆśself-regulationŌĆÖ. Until the late 1970s, medicine occupied a privileged and relatively protected position within British society. There was a belief that bad doctors were few and far between. A view prevailed that the quality of care was difficult to define and impossible to measure. There was also a pervasive philosophy that a doctorŌĆÖs performance was not the business of colleagues or management. Moreover, there was a culture in which information was neither forthcoming nor transparent to patients. In the 1980s and 1990s, high-profile cases of poor performance steadily eroded this consensus and the concept of pure self-regulation was increasingly perceived to be outmoded. Simultaneously, society had moved on. Blind deference to the professions on the part of the public had largely disappeared. Instead, the public came to see itself as the consumer of services: as such, people were entitled to expect certain standards in return for the taxpayerŌĆÖs considerable investment.
Self-regulation is still the norm in Australia and it has not protected patients from harm, as the case of "Dr Death", Jayant Patel, in Queensland attests. Will the CoAG reform process lead to health professional losing their right to self-regulate?
Posted by Gary Sauer-Thompson at 7:18 AM | TrackBack
December 20, 2006
Biomedicine, markets, biopolitics
Biomedicine is the big sign of postmodernity and the new knowledge economy in which knowledge is tied entrepreneurship, capital and the free market. Biomedicine is the future! Biotechnology is the next wave of the knowledge economy and biomedical biotechnology is seen as a key driver for the knowledge economy everywhere.
Nikolas Rose, writing in Kritokos, says that the discourse of biomedicine describes how many believe that we are on the threshold of an epochal change.
The sequencing of the human genome, it was claimed, would enable experts to read the book of life, decode the code of codes, remake Eden, usher in a brave---or terrifying---new world. Our genotypes would be read out, coded on a chip, and used to predict our fate, dignose our diseases and to personalise our medicines. New reproductive technologies would enable a world of designer babies and engineered people. Human stem cells would regenerate damaged human tissue, cure spinal injuries, heart disease, diabetes, Parkinson's and Alzheimer's. Smart drugs would enable us to engineer our moods, emotions, desires and intelligence at will. Some of the biomedical techniques cited insuch futurology are already familiar, but most are said to be 'just around the corner'. Each day seems to bring news of research that promises to increase our ability to modify, manipulate, transform our living bodily processes at will in pursuit of our secular desires.
Biomedicine is linked up with the market, as all the state governments in Australia just love biocapitalism because the biotech industry is a powerful engine of growth and change. It is a form of knowledge/power--a biopolitics.
Is biomedicine one more stage in the long history of medicalization in the sense that more and more everyday troubles are coming within the sphere of medicine, and technical fixes to misery and ill health are replacing addressing social causes of suffering. I'm not so sure. This looks to me to be something different--- more like a reshaping of our bodies to achieve perfection by improving on nature than biology is destiny; a bio-politics of life rather than an eugenics imposed by a state to improve the quality of the population; a steady reshaping of what it is to be human in postmodernity than a becoming posthuman.
Posted by Gary Sauer-Thompson at 5:05 PM | TrackBack
December 6, 2006
"the blame game"
A central issue in the urgently needed restructure of Australia's health care system is to establish models of care that prevent illness and provide early diagnosis and treatment of problems.
The health system is focused on chronic disease management and hospital care and is under greater stress due to a shortage of funding and workforce. The primary health care system is failing for a shortage of general practitioners.
Others argue that the central problem is the blame game between the states and the commonwealth, and the duplication between the two levels of government on health costing the community between $1.5billion and $4billion a year.
The rising costs of health care and a funding structure that can create incentives for state and commonwealth governments to shift costs to others and this compromises the ability of the increasingly interdependent public and private health care providers to offer the care that patients require. In the debates in the House of Representatives on health the Howard Government bashed the states for poor service delivery.
In contrast Kevin Rudd argued that the Government failed to deliver a national reform agenda in health and education, despite a $40 billion dividend from the economic boom.
Posted by Gary Sauer-Thompson at 4:08 PM | Comments (4) | TrackBack
September 12, 2006
selling off Medibank Private
So it looks as if the privatisation of Medibank Private is going to be deferred until 2008. The Howard Government has justified the sale in three ways. Firstly, that there is no good reason to retain Medibank Private in government ownership. Secondly, it would being good for the private health insurance market. This means that it would ensure more competition in the private health insurance market. Competition means lower premiums for consumers is the inference. Thirdly, Medibank's customers would benefit from greater efficiency with a privatised fund delivering lower management expenses. Private is good public is bad is the philosophy of Nick Minchin, the Finance Minister.
True, there would be increased competition, if other private health insurance companies were prevented from owning it through carving Medibank up. However, a privatised Medibank Private would need to make a profit for shareholders. Wouldn't Medibank Private then be run to maximise profits, as Julia Gillard claims? Doesn't that mean increased premiums for consumers?
You can see why there is growing public opposition to a major float of Medibank Private. The postponement measns that the proposed sale as an election issue. Labor would oppose the privatisation of Australia's biggest health fund and argue that a for-profit fund would fuel premium rises.
Posted by Gary Sauer-Thompson at 9:06 AM | Comments (6) | TrackBack
July 30, 2006
obesity
Australia appears to have lost the battle of the bulge with more than half of adults now admitting they are either overweight or obese--according to the Australian Bureau of Statistics. The Bureau of Statistics figures show that the proportion of adults classified as overweight or obese rose in the past 10 years from 52 per cent to 62 per cent for men and from 37 per cent to 45 per cent for women - giving a combined rise for both sexes from about 44 per cent to about 53 per cent.
Obesity now affects more people than smoking, heavy drinking or poverty. We are a fat nation by world standards. Despite seven reports since 1997 into obesity, Australia had failed to attack obesity as a chronic condition and Australians would continue to get fatter at a high social cost.
The modern supply of cheap, energy-rich food made it difficult for many people to temper their intake Yet the commonwealth government has said no to the regulation of the advertising of the junk food industry, which was advocated by the states. Both John Howard, the Prime Minister, and Tony Abbott, the Health Minister, say that weight control is a matter of personal responsibility and does not require govenment regulation or intervention.
Is this benign neglect?
If weight control is a matter of personal responsibility means that consumer responsibility in health promotion and prevention is now accorded a central role in achieving affordable care, then what is needed is creating an an environment that favours healthy weight. One shot solutions---ie., a single cause-single remedy public health problem---are not going to work because of the complexity of the causes--food, lack of excercise, tv advertising, urban design. For instance, the places where children's most important food choices are made (school and family) need to be targeted.
Paul Goss argues that fatty foods shouls be banned in canteens, school report cards would proide information on a children's body mass index, parents and childrern would recieve far moe educaion about appropriate eating and governments would provide more in-school and after school exercise opportunities.
Posted by Gary Sauer-Thompson at 7:12 PM | Comments (0) | TrackBack
July 5, 2006
obesity, market failure, neo-liberalism
Ross Gittins had an article on obesity in The Age a week or so ago. Looking at it from an economic perspective he argues that the fundamental causes of the developed world's obesity epidemic are economic, that it is a case of market failure, and that government intervention is required.
As Harry Clarke points out at Kalimna the 'extent to which you want the state to intervene in people's lives is a major issue distinguishing different camps of political philosophy.' Samuel McSkimming over at Catallaxy says that Gitten's argument for state intervention is incoherent. Is it?
So let us look at Gittin's argument, and then we can see how far the debate has progressed beyond the idealogues saying that privatising socalised medicine is the grand solution or that nothing should be done. Gittins says that the obesity "epidemic":
...constitutes a damaging side effect of technological advance and economic growth....the sudden surge in weight seems to be better explained by developments on the consumption side. According to a study of obesity in America by two economics professors at Harvard, David Cutler and Edward Glaeser, in the 1960s, the bulk of food preparation was done by families that cooked their own food and ate it at home. Since then, there's been a revolution in the mass preparation of food. Technological innovations ŌĆö including vacuum packing, improved preservatives, deep-freezing, artificial flavours and microwaves ŌĆö have enabled food manufacturers to cook food centrally and ship it to consumers for rapid consumption. This greatly reduced the "time cost" of food production, both at home and commercially.
That is about right. The way we prepare and consume food has changed with industralization in late modernity ---today we eat more snacks, and these are more likely to be mass-produced, high-kilojoule (that is, high-fat, high-sugar) treats and as processed snacks from the supermarket.
Gittins then highlights the consquences for public health:
I need hardly remind you that our growing obesity problem has serious implications for our health and the cost of health care. It's leading to increases in type 2 diabetes (what used to be called late-onset diabetes until kids started getting it), heart disease, several types of cancer, musculoskeletal disorders, sleep apnoea and gallbladder disease.
That is about right too, in spite of those who say that junk food is just a matter of personal taste or that fat is okay.
Gittins then makes a move that many would disagree with. He says that what we have here is an unusual but serious case of "market failure" as a result of 'capitalists using all their wiles to flog their food and make a quid is major social and economic dysfunction.' That inference strikes me as about right. As the consequence is rising health costs, then prevention is the best health policy to contain the health costs. So governments have an interest in doing something to prevent obesity. Gittins then makes the classic social democratic response to market failure. He says:
When market failure is demonstrated, and is known to have serious consequences, the case for government intervention is established. One obvious corrective would be to limit the use of advertising to induce over-consumption ŌĆö particularly by children.
That is a limited response for sure. You could also change the food sold in the tuckshops in public schools, or regulate to put health warnings on the fatty foods. Gittins concludes that 'there's ample precedent for government intervention to protect our health against the excesses of an unfettered market: tobacco control (pricing, advertising and promotion restrictions, smoke-free restrictions), road trauma minimisation (mandatory seat belts, speeding and alcohol restrictions) and injury prevention (restrictions on firearms, fireworks and safety regulations).'
The neo-liberal response is to deny market failure and the usefulness of government regulation. Thus Chris Berg, writing in reponse to Gittins in The Age, disputes the conclusion that government intervention is needed, as it is a matter of individual responsibility. He says that we are getting heavier (not necessarily fatter) and that:
Part of this is to do with the composition of our diet. But most of the recent growth in weight is not directly attributable to our food. A study by the economists Darius Lakdawala and Tomas Philipson found that only 40 per cent of weight gain since the 1970s is due to changes in diet. Rather, the large part of our weight increase can be attributable to changes in lifestyle and work practices.Contrary to what Gittins has argued, this is not an opportunity for government to intervene.
What about food? Or encouraging companies and bureaucracies to help their workers to increase their exercise during the lunch hour?
Berg's response is to say that government regulation doesn't seem to work, (citing Sweden), that the market is remarkably good at educating people on the negative consequences of their decisions, and that consumers are becoming more aware of the consequences of fatty and unhealthy food. A few books do not counter the advertising of the junk food industry. As Harry Clarke points out information is a public good so we can expect it to be underprovided unless it services a private interest. Thsi avoids the implication of the libertarian argument that those consumers who get fat are flawed--stupid; ie., a small minority of pathetic fools.
Berg concludes the neo-liberal case:
The notion of a government regulating to protect people against obesity used to be unthinkable, used as a parody of anti-tobacco legislation. Unfortunately, it shows us how far the political debate has moved from personal responsibility to government responsibility. But is there a clearer area in which individual responsibility must take the fore than when choosing what we eat? Government regulation is not the solution to the obesity crisis.
So if its all a matter of individual responsibility, then how do we deal with junk food, fat people and lack of exercise and so prevent called late-onset diabetes heart disease, several types of cancer, musculoskeletal disorders,with their implications for the cost of health care? We should be concerned because they cost all of us more in health costsŌĆÖ. A substantial component of health costs will be taken up with obese people with diabetes.
Samuel McSkimming at Catallaxy adds to this neo-liberal position by saying that:
My general view is that provided consumers face the correct price signals (and arguably they currently do not), they can do whatever they like - including smoking/drinking/eating themselves to an early grave.
There is no market failure.The problem from a liberal perspective is that though we have the failings (self-harm) of a significant minority of the population, the rest of the population are able to control their desires. So though there is a market externality, there is no market failure, because those who rarely eat junk food suffer no negative effects. Hence the problem for the libertarians becomes one of fat people getting cheap donuts.
Why not introduce a tax on junk food as has been done with cigarettes? The libertarian response is that you impose costs on people who consume the food occasionally, which means that in effect, those of us who like the occasional indulgence (eg., McDonalds or Hungry Jacks as a treat) are subsidising those with no self-control. So? They can choose to eat something else than McDonalds, if they do not want to pay extra for their luxury indulgence.
I do not see that the libertarian case against state intervention has been made. It is a case of both individual and government responsibility, not an either or. The question then becomes, what kinds of intevention are best?
Posted by Gary Sauer-Thompson at 8:28 AM | Comments (3) | TrackBack
May 23, 2006
Gillard on politics and health policy
In launching the Tim Wright (ed.), Time for Change book at the Paperchain Bookshop in Manuka, Canberra, Julia Gillard, Labor's health spokeswoman, said that the reporting of politics tended to focus on the personalities at the expense of promoting discussions around public policy. She said:
...politics has been narrowed down to a political contest with personalities....there is a sense of who won, who lost and who made the play of the day. But this is not politics at all---the real stuff of politics is a contest of values and ideas about how to make a better nation.
This is the politics as a sporting contest view of politics of the Canberra Press Gallery that is based on reading minute signs and moods:

Allan Moir
The Sydney Morning Herald reports that in her chapter in the book Gillard argues for fresh thinking in health policy and that progress is being paralysed by a conservative Howard Government's resistance to change.
Gillard says hospital delays, inadequate services for the aged and mentally ill, and a health system straining under layers of administration show the need for a thorough rethink of health. She then argues broadly for a more patient-focused system that places more emphasis on preventative care to reduce chronic illnesses, and rebuilds what she calls the "public realm".
Gillard says that Australia should be doing more to combat diseases like diabetes, cancer and cardiovascular disease, all of which were at least 50 per cent preventable.This could be done by developing population health measures to ensure that people did not go to the doctor when feeling ill but have appropriate continuing contact to manage their health, identify risk factors and to be screened to help early diagnosis.
She says that if we are to surmount the situation of health services under pressure, overworked staff and governments shifting blame, the we must open our minds to new ways. Rather than addressing poor co-ordination and service delivery, or barriers to alternative types of care, spending had been focused "on short-term political fix-its".
Posted by Gary Sauer-Thompson at 4:36 PM | Comments (6) | TrackBack
May 5, 2006
addressing obesity
Tony McMichael, director of the National Centre for Epidemiology and Population Health, at the Australian National University has an interesting op.ed. on obesity in todays Sydney Morning Herald. It is one of the better articles on obesity in the corporate media.
McMichael states what we know: the proportion of overweight and obese people in Australia has doubled in the past quarter of a century, and now includes more than half of all adults; the proportion among schoolchildren, about a quarter, has risen even faster. He then argues that 'this trend, evident in populations around the world, signifies that something fundamental is changing in how we live. Our daily energy balance is out of kilter.'
He notes that much of the public discussion mostly focuses on strategies to intervene, correct and counsel at the personal level, either in terms of "fatness genes" or personal behaviour, and then critiicizes this approach.
The "fatness gene" approach he says:
might explain why some people become obese. Such reports reinforce the idea that solutions lie with correcting or compensating for individual biological abnormalities. In like vein, many view the basic problem as one of aberrant individual behaviour. The Health Minister, Tony Abbott, argues that preventing weight gain is essentially a matter for personal and family discipline, and not a matter for governmental policy.
The flaw with the personal approach - both biology and behaviour--- is that this individual-focused thinking misses the point, which is the population perspective.
McMichael argues that though genes and behaviours are very relevant, in relation to the rise of obesity their main importance is at the population level, not at the individual level:
If we cannot understand that the problem has a systemic source that arises from recent radical changes in our way of living, in human ecology, then society is unlikely to find effective solutions.Our way of living is no longer attuned to our basic biology....Inadvertently, then, we have created an evolutionary nirvana in which, at last, abundant (and energy-dense) food is within easy reach and its purchase or acquisition requires little exertion.
Being overweight is one of the several main new penalties of modern urban ecology. As McMichael argues that as, such an environment is a man-made cultural artefact, creating an environment far removed from the conditions that shaped our biology and psyche, so it is not surprising that there are some health penalties.
He locates this in the public narrative of governing the health penalties of urban-industrial life (the airborne and waterborne infections, including tuberculosis, measles, diphtheria, cholera and other diarrhoeal diseases) which have largely been controlled, via the joint processes of public-health intervention and social modernisation:
Two of the greatest health endangering consequences of the late-industrial urban environment are, first, overweight as a manifestation of this radical shift in human ecology and, second, the increasingly huge contribution of the world's cities to greenhouse gas emissions with all that they portend, via climate change, for future risks to safety, health and survival.
McMichael rightly argues that solving such problems requires well-informed, imaginative population-level strategies. That is not nanny statism; it is enabling statism:---enlightened, government-supported, collective action.
Posted by Gary Sauer-Thompson at 7:00 PM | Comments (0) | TrackBack
April 28, 2006
health insurance
This week's announcement of the sale of Medibank Private by Nick Minchin, the Finance Minister, did not tell us much that we didn't already know. It will be a trade sale or a public float, most likely a trade sale. The sale was bound to happen, given the anomaly of the government owning a private health insurer and being a regulator of the health industry.
However, it does not represent much of a reform step to a healthier Australia, does it? Is that why it was dressed up with the expansion of hospital cover to cover outpatient and out-of-hospital services, chronic care management for conditions such as diabetes and asthma, and insurers being able to cover disease prevention measures.
Contrary to the claims by Tony Abbott, the Health Minister, I cannot see that this sale will prevent health insurance premiums continuing to rise by more than inflation. Whilst inflation is around 3% per annum, health insurance premiums increases range from 5.7--7.4%. How does the sale represent increased consumer choice?
What is not generally mentioned in this is that for every additional dollar of premium that health funds collect 30cents is paid by the government in the form of private health insurance rebate. That rebate is designed to encourage the trend to private health insurance cover.
In an entry for 2004 in the Latham Diaries Mark Latham states the ALP's opposition to the private health insurance rebate:
A good meeting this morning with Gillard's health experts, Stephen Duckett and Hal Swerissen. We have worked out a way of dealing with the despised private health insurance rebate. We need to kill it slowly; adopt the strategy Howard and Woolridge used for their attack on Medicare, dismantling it slice by slice. (p. 267)
Why would you slice it bit by bit?
Well, since the rebate applies to everyone it works to favour those who can afford to take private health insurance--those high income households who would have taken out private health insurance anyway, if there was no rebate. The other side of the picture is that the uninsured on low incomes are disadvantaged: they have to pay taxes from which the rebate is paid, face a reduced level of services at underfunded public hospitals.
Posted by Gary Sauer-Thompson at 5:13 PM | Comments (4) | TrackBack
April 6, 2006
Finally, some progress
It's taken a long time, but finally the Commonwealth has announced a $1.8 billion, five-year plan to treat mental health. It includes more respite care, mental health nurses, community-based programs and patients with mental illness will be able to get care from psychologists at a much lower cost than the current $120 per hour under a big expansion of Medicare. The plan turns around decades of neglect in mental health care after the de-inistutionalization process of reform.
John Mendoza, chairman, of the Mental Health Council, observed:
in the same way that the States and Territories got together to deal with aged care, and moved many of the people who were in long stay beds in our hospitals into appropriate aged care settings, there's an opportunity to move at least 30 per cent of those patients who use acute care, psychiatric beds, into longer stay facilities in the community. They don't exist now, they have to be funded to be built, they have to be funded to be staffed and resourced, and I think that's a discussion that has to happen between the Commonwealth and the States. I don't think the States can do it on their own.
So reform progress depends on whether the Commonwealth's move is matched by the states and whether together they can deliver a system of appropriately balanced hospital and community care.
Posted by Gary Sauer-Thompson at 4:04 PM | Comments (1) | TrackBack
April 5, 2006
privatising Medibank Private
So the Howard Government is going to privatise Medibank Private. It will be flogged to ensure the best possible sale price for the Commonwealth.
What then happens to the public interest of ensuring better health outcomes for Australians? Does not the sale mean that premiums will increase? Who is to ensure that there will be competition between pirvate health insurance funds? Who is there to force premiums down?

Fat
We have a highly subsidised private health industry that delivers a poor health product without a strong regulator. Who will now keep the private health insurers honest? Who will now consciously steer the health market in a given direction to achive better health for consumers? Which fund will now act as a health broker using its market power to purchase cost-effective services for members at the most competitive price commenssurate with account quality and safety considerations.
Jack Waterford in the Canberra Times outlines the possibilities of the sale that make the market less not more competitive.The first possibility is this:
Suppose, for example, that one of the bigger existing health funds took over Medibank Private, with its three million contributors and 29 per cent of the market. Would greater competition - and lower premiums - be more likely with a single player having half the market?
I presume the ACCC would say something about that, would it not? The second possibility is:
Suppose instead that the Government did something some ministers have mused aloud about - breaking up Medibank Private, perhaps into regional chunks. Would that improve its economies of scale, and lower administrative costs presently running significantly below those of its competitors?
That is the dismembering option as the other funds may be interested in stripping off parts of Medibank Private in order to improve their own national coverage. That leaves us with 3 health funds controlling 80 per cent of the market. The second possibility is not likely to produce improved performance of the private health insurance.
The third possibility is:
Suppose it were bought up by a merchant bank. Machealth would be too clever to run it into the ground, but how much temptation would it face to enhance the "value" of its product by shedding, through cost structures, the expensive customers? And given the history of supine responses by health ministers to demands for premium increases - in spite of increasing general taxpayer subsidisation of private health care - how confidently could one expect hard questions to be asked of the big end of town?
None of the possibilities are reassuring are they?
Posted by Gary Sauer-Thompson at 4:50 PM | Comments (6) | TrackBack
March 31, 2006
privatisation by stealth
I've just returned to Adelaide after spending the day walking the federal Parliament in Canberra talking about the direction of health care reform and the problems caused by an expensive user-pays health system:
Then on the shuttle flight home I read that the solution to the health care crisis by Queensland Health is privatisation---aah you can smell the hand of Treasury, can't you. David Gilchrist, writing in the Courier Mail quotes State Opposition health spokesman Dr Bruce Flegg, to the effect that:
it is likely that Queensland Health will increasingly provide health infrastructure while private contractors provide health care, training and research services....the result has been higher healthcare costs and, in some cases, the removal of services from public access....The Government has got itself out of a political fix by throwing some money at health and getting somebody in the private sector to bail them out.
So the Beattie government is creating a private system at the expense of expanding the capacity of the public sector and so deliberately choosing to go to a system that is more expensive to administer.
Posted by Gary Sauer-Thompson at 7:58 PM | Comments (1) | TrackBack
March 5, 2006
a political joke
Premier Peter Beattie in Quensland announced last Thursday that Queensland's health system had "turned the corner". It's a joke isn't it.
How can such a dysfunctionalsystem be turned around so quickly with a promise of cash and more doctors from full feeing paying courses? Secondly, have not voters lost confidence in the Beattie's Government ability to "fix" Queensland Health? The glossy Team Beattie, who basically see themselves as administrators and managers, have moved into election mode.
Are we not also losing patience with Tony --'-my job is to fix the problems'--- Abbott, and his resistance to health care reform, and his unwilllingness to make the shift from linking government spending decisions to looking after doctors to spending money to look after patients?
We have problems: allocative inefficiency, poor use of information technology, lack of competition, cost shifting and buck passing, narrow models of health care, medical dominance, too much focus on chronic disease in hospitals etc. We have an ageing population and a disintegrating public health system. Where's the fixer? Is it not a myth--that a health minister can "fix" the problems in the health care system? How can we fix a situation where 2 out very 3 Australians court diabetes and heart disease by being overweight?
Even the Australian Financial Review is argues that the problem solving approach of the fixers is wrong:
Health care ashould be as much about encouraging people to adopt healther lifestyles as about treatign their ailments. The present model where---where doctors and hospitals keeping meeting demand instead of trying to stem it at its source---doesn't address this need.
Of course the centraliists, such as Andrew Podger, the former Canberra health bureaucrat, want to eliminate the states with commonwealth providing services direct to regional health care purchasers. How are you gonig to address overweight and obesity in the Australian population without the help of the states in a federal system? It's bureaucrat dreaming.
Posted by Gary Sauer-Thompson at 5:25 PM | Comments (0) | TrackBack
February 28, 2006
unhealthy lifestyles
There is little sense that the changes we need in the health care system are happening. There is a sense of stasis.
The graphic cartoon is one reason why the focus of the health care system needs to shift to preventative health and primary health care: Australians are getter fatter:
Overweight indicates how the pressure and burden on our hospitals from chronic illness can be lifted if we all took more responsibility for our own health through changing what we eat and doing more exercise.
Alas, no one owns the territory of primary care, and it is deeply contested by the different health groups.
Australians are getting fatter. The recently released Australian Bureau of Statistics national health survey, ,found 62 per cent of men and 45 per cent of women were overweight or obese. However, only 32 per cent of men and 37 per cent of women saw themselves that way, despite millions spent by state and federal governments on promoting a health lifestyle.
This indicates that only about 1 in 3 adults believe themselves to be overweight or obese, yet more than 1 in 2 adults are overweight or obese. If some adults ... parents... believe themselves to be a healthy weight when they are not. How can Australians get it so wrong?
Posted by Gary Sauer-Thompson at 6:47 AM | Comments (0) | TrackBack
February 23, 2006
questioning medical power
And so the undermining of the power of the medical profession by the government has begun.
It's taken the initial form of the state health ministers appealing to the ACCC to review the Royal Australasian College of Surgeon's ability to decide how many surgeons are trained. The College---a doctor's club---is seen to be limiting the number of trainee surgeons. They control the numbers so it is not just a question of a lack of funding for trainee posts. The College is a monopoly controlling access to a profession. It's a closed shop that needs to be busted open for the public good.
How to do this is the problem? It is going to require some heavy lifting to remove the closed shops and monopolies throughout the health system. Bringing in other competitors is the answer. Who then would provide high quality training for surgeons? The universities could, if they worked together says the editorial in the Australian Financial Review:
The good news is that it is not up to the ACCC to bust open this particular closed shop. The regulator's authorisation permits the monopoly, it doesn't stop anyone else entering the market. When the authorisation was renewed, the ACCC noted with evdent relief that high-quality alternative systems for training surgeons could exist...all it would take is a group of major universities to band together and the club of surgeons would no longe rhave a monopoly.
They would need help to break the monopoly. Will the state governments do that? Or will they and the federal government baulk at taking on the vested interests of the AMA and the medical colleges.
Posted by Gary Sauer-Thompson at 1:11 PM | Comments (2) | TrackBack
February 13, 2006
junk food as sin?
We are living longer and getting fatter. Obesity is seen to be the fastest growing illness in Australia. People even talk about obesity in terms of 'epidemic' and toxicity.
One of the key issues in health care reform is shifting the focus to primary health care and to prevention. Obesity is a good example of the need for this approach--good diets and fitness prevent diabetes, heart disease and blood clots. if not prented then then we take up for weight loss medication and, if that is not successful, then bariatric surgery where your stomach, usually the size of a large melon, is reduced to the size of your thumb. The pouch in the uppermost part of the stomach, is literally stapled off from the rest of the stomach.
Are we not repulsed by fatness? Is it not held to be morally reprehensible to allow yourself to become fat? Do we not come to loathe ourselves if we are fat. It's an individual responsibility issue conservatives say. I choose to be fat. Yet we are surrounded by advertisements that tempt us to become fat.
Maybe we should start treating junk food the way do cigarettes and cigarette advertising and use the money to fund nutrition and exercise programs.
Posted by Gary Sauer-Thompson at 6:47 PM | Comments (1) | TrackBack
February 10, 2006
Canberra watch: Gillard on health
Though I haven't been in Canberra this week I've been watching the happenings in Parliament---noting the Nationals ongoing disintegration, the festering Coalition tensions, the politically confused attack by the ALP in taking the fight to the fight to the Government over the kickbacks by the Australian Wheat Board Kim Beazley's backwood looking speech to the National Press Club, the debate over RU486 and the way Simon Crean is being allowed to hang out to dry.
The only bright spark was the speech Julia Gillard gave on health care to the National Press Club on Wednesday. it was tightly focused on prevention: on preventing the emergence of an American-style health system; adding prevention to the debate involving population, participation and productivity; and placing prevention at the centre of the health care system.
The implication, as Gillard, was quick to draw, is to:
"...abandon the language of post-war policy that puts a brick wall between 'social' policy and 'economic' policy and accept that there is an inextricable link between the health of our people, the health of our health system, and the health of our economy."
Rightly said. The majority of spending in the Australian health system still goes on treating existing problems when they become chronic conditions--billions are spent on spent on managing diseases rather than preventing them in the first place. Australia really does need an an integrated primary health care and prevention strategy.
So how does Gillard propose to do this?
She says that in an earlier speech to the National Press Club in April 2004 she mapped a pathway:
I outlined how Medicare fee-for-service fails to provide the right incentives to encourage regular checkups and screening and the provision of health advice.The problem is that at the moment, the only time a GP gets paid is when they see a patient, and the only time they see a patient is when the patient is sick. The proposed new Medicare payment for wellness checks falls in to this category. If you go to the doctor - fine. But there is still no incentive in the system for the doctor to look at his or her patient load and come and find you for a wellness check.
What is required is a proactive component. Which is? Another limitation is the concentration on GPs's delivering health care. Wjere is allied health?
Posted by Gary Sauer-Thompson at 3:11 PM | Comments (2) | TrackBack
January 25, 2006
medical politics
I see that John Dwyer, Emeritus Professor of Medicine at the University of NSW, is having a go at alternative healthcare, in the name of "evidence-based medicine" and its potential for protecting consumers from spurious health claims. He has been watching the TV coverage of the Australian Open tennisand has found it to be a frustrating experience. He says:
The constant reminder by another Australian Open sponsor, Medibank Private, that, in an effort to boost falling membership numbers, it (as do many other private health funds) provides coverage for a range of "alternative" therapies, demonstrated to be of no benefit, is also disturbing. By so doing, these insurers directly, and the Australian Government indirectly, provide an imprimatur for nonsense techniques such as reflexology, homeopathy, iridology and various massage therapies.
Now I regularly use chiropratic care, massage, fitness clinic, and take diet advice to help manage my stress levels, reduce my weight, and ensure my wellbeing and quality of life. So I take exception to Dwyer's phrase ' "alternative" therapies, demonstrated to be of no benefit'. It is far too sweeping in its characterisation of the bogus health-care market.
Moreover, Medibank Private has moved in this direction because of consumer demand. They are shifting from GP focused primary care to a wellness conception of health care. Modern life is stressful and exhausting and we consumers are looking for ways to cope with that and we are in need of good advice.
The thrust of the Dwyer article is a criticism of the misleading claims about the products of companies such as Nature's Own and Blackmores. It is constructed around consumer deception without ever mentioning the misleading advertising claims by Big Pharma for its pills. Isn't there a profitable, exploitation of the well and the ill on both sides of the pill popping medical/non-medical fence?
I support Dwyer's suggestion that the Therapeutics Goods Administration should be beefed up and fully resourced and its powers increased. I cannot see that happening. Consumer protection is not a big concern of the Howard Government.
Posted by Gary Sauer-Thompson at 7:58 AM | Comments (1) | TrackBack
January 20, 2006
reforming the health care system
The Productivity Commission has just released its report about refoming Australia's health workforce. Health care reform is sorely needed in Australia:

Lethbridge
It addresses the issue of the healthcare workforce because there are workforce shortages across a number of health professions (especially noticeable in rural and remote Australia) and, with developing technology, growing community expectations and population ageing, the demand for health workforce services will increase while the labour market will tighten.
Hence Australia has an increasing workforce shortage that cannot be meet by doctors, no matter what the AMA spin says about a doctor is a doctor is a doctor, or that Australians want quick and affordable access to a doctor, not a doctor substitute. The AMA is just another bully-boy trade union into restrictive trade practices. Australians turn to non-medical health professinals because they offer a different model of care to that provided by the GP. Competition and consumer choice is what is needed.
The GP shortage means the end of medical dominance, the patch protection by the AMA, and the GP acting as the gatekeeper to the healthcare system. Will the Howard Government have the courage to further that process? It all depends on who is the health minister and why they have been put in the job, doesn't it. Will a reformer be put into the job? Or a free marketeer? Or a timeserver beholden to the Canberra health bureaucrats?
The Productivity Commission, to its credit, does point in the right direction. It says that:
It
is critical to increase the efficiency and effectiveness of the available health workforce, and to improve its distribution.The CommissionŌĆÖs objectives are, therefore, to develop a more sustainable and responsive health workforce, while maintaining a commitment to high quality and safe health outcomes.
The reason fo the AMA's negative response is the Commission's proposal to improve funding-related incentives for workforce change through:
...the transparent assessment by an independent committee of proposals to extend MBS coverage beyond the medical profession; the introduction of (discounted) MBS rebates for a wider range of delegated services; and addressing distortions in rebate relativities.
That opens the door for allied health professionals to play a more substantive and independent role in the provision of quality and cost effective health care.
Posted by Gary Sauer-Thompson at 10:58 AM | Comments (2) | TrackBack
January 17, 2006
Queensland health #3
The emergency department in Queensland's Caboolture hospital on Brisbane's northern outskirts has been closed. The reason? A statewide doctor shortage.
Unsuprisingly, the Beattie state Labor government denied the closure up to the very end; then the Health Minister shifted the blame to his health department for providing him with incorrect information. Canberra is then blamed for the doctor shortages in the state. Where then is the Minister's responsibility in all of this?

Lethbridge
Closure of the hospital's emergency department spells tragedy for road accident victims and others requiring emergency treatment in the area. They have to be transported to other hospitals or flicked over to the local GP's. Crisis situations and newspaper headlines then give rise to stop-gap policy on the run.
It will happen again at another hospital across the state. The problem is systematic as the doctor shortage in the StateŌĆÖs hospitals are the culmination of many years of staffing difficulties, due to the failure of government (both Federal and State) to train, employ and retain doctors to support QueenslandŌĆÖs burgeoning population. So doctor numbers are simply too low to meet patient demand. Around 20 public hospitals in Queensland have been affected by shortages that have centred on emergency and maternity departments.
Posted by Gary Sauer-Thompson at 7:43 AM | Comments (2) | TrackBack
January 16, 2006
hospital deaths: treat them like road deaths
There is a consensus on what kind of reforms Australia's buckling health system needs. Those needed include significant integration of federal and state responsibilities; finding alternatives to hospital treatment since the rate of hospitalisation in Australia one of the highest in the world; and breaking open the doctors' closed shop to allow more health to be delivered by other professionals.

Bruce Petty
The preferred reform pathway of the centralizing administrators is the commonwealth taking full financial responsibility for healthcare. That magic bullet is not politically feasible under the Howard Government as John Howard has consistently ruled it out.
What is rarely mentioned in the reform talk od the centralizing administrators is the number of hospital patient deaths. Yet these number around 5000 per year due to unintended errors and accidents. This is more than road deaths (around 3000 p.a), yet government agencies work to prevent the disclosure of death and injuries in Australia's hospitals due to poor or negilgent medical practices.
Strange isn't it.
The bureaucratic silence I mean.
 It's a case of hiding the problem. It is a public problem though, just like road deaths, and consumers of health care services, as well as those who work in the health system, are deserving of a safer hospital system.Yet it appears that injuries and deaths will continue to increase in public hospitals and that reform moves for a national mandatory requirement to report doctors to medical registration boards, health departments and consumer groups will continue to be blocked.
It's a case of hiding the problem. It is a public problem though, just like road deaths, and consumers of health care services, as well as those who work in the health system, are deserving of a safer hospital system.Yet it appears that injuries and deaths will continue to increase in public hospitals and that reform moves for a national mandatory requirement to report doctors to medical registration boards, health departments and consumer groups will continue to be blocked.
Aren't citizens entitled to be informed of important health care information without unreasonable delay? Indirectly, we citizens own most health care research in Australia because it is predominantly funded by our taxes and it is our health that is at stake. Should not health reform include a culture of honest reporting?
If it is mandatory for hospitals to report fatal and serious illness sustained as a result of rare and preventable circumstances, then it should also be mandatory for the Minister to reveal this information to the public. Health deaths shoudl be treated just like road deaths.
Posted by Gary Sauer-Thompson at 11:19 AM | Comments (0) | TrackBack
January 12, 2006
health reform anyone?
It is now widely accepted that the neo-liberal efficiency approach to Australia's health system has 'squeezed the system too far' in its search for efficiency savings, and it has been too slow in responding to increased demand for health care by providing more primary health care services outside of our hospitals. The health care system is hospital-centric.
The assumption underlying the neo-liberal mode of governance is the seductive notion of progress where an industrialized Australia pumps more wealth in one end of the pipeline and more welfare flows out the other. Yet, what we have discovered with a decade or so of solid economic growth is that you can have more wealth and more people exluded from welfare. This indicates the import of social justice.
Is the shabby treatment of those who are mentally ill the price of progress that must be born? It looks increasingly likely, doesn't it.

Alan Moir
Around one in five Australians will experience mental illness in some form or another. Around 27 per cent of all health-related disability is due to mental illness, and that a staggering 60 per cent of disability among 15 to 34-year-olds is due to depression, anxiety, alcohol and substance abuse, manic-depressive illness (bipolar disorder) or schizophrenia.
The response is pretty poor.
If we suffer from depression, we are often told to 'snap out of it!' or 'that we have nothing to be depressed about'. The tacit assumption is that we choose to be mentally ill, just as we choose to be poor and excluded. It's a lifestyle option.
You don't need to go to line up at hospital to be treated for depression. You need good primary care. That doesn't just mean drugs. It means psychological help and support for families and carers of loved ones suffering mental illness.They carry the burden of the lack of access to basic medical, psychological and social services for those with mental illness, despite a decade of promises by all governments to lift the quantity and quality of mental health care. Hence the basic failures in the system occur on a daily basis and cause a lot of suffering.
I cannot see the full Commonwealth takeover of the financial responsibility of the health system would solve. This Many centralists see it as a feasible option. However, the Commonwealth has been as slack as the states in helping address the basic failures in mental health. It hides behind the fiction that it is the states problem, even though all Australian Governments initiated the National Mental Health Strategy in 1992 to address decades of neglect and assure the rights of people with mental illness.
Posted by Gary Sauer-Thompson at 7:04 AM | Comments (2) | TrackBack
January 4, 2006
big pharma makes its moves
I see that Medicines Australia--- the US pharmaceutical firms---are starting to have a go at the Australian PBS scheme by using the recently signed Australia-US Free Trade Agreement. It did not take them long to make a start to begin to wind things back behind closed doors.
Big Pharma does not like reduced prices for their exclusive drugs. They want increased prices to make ever bigger profits. Hence their hostility to the measures introduced this year to cut the price of new generic medicines by 12.5 per cent. Kieran Schneemann from Medicines Australia said that cutting the price of new generic medicines:
"...was a difficult policy for us. It forces the prices of medicines down ŌĆ” and we are concerned in the future as this policy continues to roll out that it will impact on the value of innovative medicines and it may in time prevent some new innovative medicines coming to Australia."
These are old drugs at the end of their life. It is where the big profits are made. Big pharma is not going to give this up. The generics have to be contained so as to protect their monopoly rights to their exclusive drrugs.
Australia cannot expect much sympathy from the US government on this issue. The Bush administration consistently acted to support the interests of Big Pharma in the negotiations around US Australia Free Trade Agreement last year.
Bush basically repeated the big pharma line when in Australia:
"Our research and development costs are enormous, and we need to cover them somehow. As 'research-based' companies, we turn out a steady stream of innovative medicines that lengthen life, enhance its quality, and avert more expensive medical care. You are the beneficiaries of this ongoing achievement of the American free enterprise system, so be grateful, quit whining, and pay up."
Since prescription drug costs are rising so fast, the federal government is particularly eager to get out from under the burden of the PBS by shifting costs to individuals. The result is that more people have to pay a greater fraction of their drug bills out of pocket. Increasingly, many cannot afford them.
Posted by Gary Sauer-Thompson at 8:40 AM | Comments (6) | TrackBack
January 2, 2006
a future pathway of health reform
In the Review section of the weekend Australian Financial Review there is an article entitled 'The World to Come', which has been downloaded from Foreign Policy. The article consists of the views of leading thinkers on what won't last the next 35 years. One piece, by Graig Mundie, a senior vice-president and chief technical officer for advanced strategies and policy at Microsoft, address health care reform in the form of changes to the doctor's offices.
It's an important topic in Australia given this scenario:

Bruce Petty
An earlier post on this scenario.
Mundie rightly says that a crushing burden isincreasingly being placed on national health-care systems, and that governments will:
"..soon be forced to confront a complicated and inefficient system that focuses too much on managing disease when it arrives and not enough on preventing people from getting sick. A critical step in reforming the system will be making visits to the doctor's office as a last resort rather than a first step."
That is beginning to happen in Australia under Treasury governance. We are on the threshold of reconsidering the importance of primary health care, and wellness is becoming a part of medicalspeak.
However, Mundies' focus, as a Microsoft organization man, is on medicine and technology. So what's he pointing to? What is the pathway of health care reform as envisioned by Microsoft?
Mundie says that the web is already allowing patients quick access to quality health information once dispensed only by white coats. He adds:
Soon, patients wil access customised health plans online. Diagnosing and treating many everyday conditions will be as simple as despositing a drop of blood in a machine and, within moments, having the computer tell you what you have and how to get rid of it.
That is happening slowly in Australia, very slowly. The slowness is in sharing e-health records due to the medical profession's tardiness in making a patient's health information accessible to non-medical professionals or even to the patient.
Mundie argues that doctors (GP's) won't be obsolete. They:
...will spend more time assessing options for preventative action and less time sheperding patients through their offices. Doctors will increasinlgy rely on highly personalized treatments--such as new drugs target specifically to personal needs, or even nanomachines that attack bad cholestrol and or eliminate tumors too small to detect today. Specialsts in turn will be free to focus on highly difficult procedure and push the frontiers of health care.
This is a high-tech interpretation of health care reform, much favoured by the Americans. Preventative health care is also about wellness: keeping us out of hospitals and helping us managing lifestyle illness (eg., obesity) through diet and ecercise. We don't need new drugs or cutting edge surgical procedures to address obesity.
Posted by Gary Sauer-Thompson at 8:50 AM | Comments (3) | TrackBack
December 30, 2005
rising costs of health care mean...
I see that Australia's health insurance funds are pushing for another round of premium rises of up to $200 a year: This time the funds have applied for price increases beyond the 5 per cent to 7per cent hikes of recent years for some policies. The current increase is about double the inflation rate for the fifth successive year. We appear to be on an escalator of steadily rising health costs year in and year out.

The steady price increases ensure that private health insurance is becoming less attractive. They offer a limited range of services that adress wellness or healthy human functioning.
Private healh insurance is currently subsidised with a 30% tax rebate, costing taxpayers $3 billion a year. This subsidy is underwriting an uncapped and increasingly costly use of private health care. That means an increasing two tier health system doesn't it. Which is what the Howard Government wants--to shift Australians away from a public health care system that becomes a residual, stop gap system for the poor. Many in the Government want to encourage more people to take out private health insurance and not rely on state provision of health care, thus giving more scope for tax cuts. That is the neo-liberal approach to health care reform isn't it?
So where does the ever rising premium for private health insurance leave health care reform?
I cannot see much reform happening under Tony Abbott. He's done his political job as Health Minister:-- he neutralised Medicare as a election issue, and he succeeded in placing the ALP on the backfoot with its Medicare Gold proposal. Time for a new face, new energy and more reform that is different from pushing citizens into expensive private health insureance.
Will that happen in the new year cabinet reshuffle of the Howard Government?
Update: 31 Dec.
One reform pathway is to make "empowering patients to play a bigger role in choosing where and who provides them with their health service" a reality that is underpinned by the twin pillars of competition and plurality of provision. Choice in the marketplace depend on having good information and the skill of understanding and choosing between options whose probable consequences cannot be measured or even known. How do we do that?
Another reform pathway is the big turn to complimentary and alternative medicine. Women in their mid-20s to mid-40s, with higher income and education and living in the city, are the biggest users overall of alternative medicines and therapies, with most people using them to promote general good health or wellbeing.
Posted by Gary Sauer-Thompson at 5:04 PM | Comments (2) | TrackBack
December 21, 2005
social health atlas of SA
A social health atlast on SA has been released by the University of Adelaide's Public Health Information Development Unit. This is the region's first social health atlas and it was prepared for the South Australian Department of Health.
The argument from the interpretation of the data is simple. Half of the SA's population lives in regions with alarming health inequalities, leading to higher rates of obesity, cancer and early death.
The Atlas confirms what we suspected in terms of the geographial spread of inequality.The most disadvantaged people in the Central Northern Adelaide Health Service area (Playford, Salisbury, Elizabeth and Port Adelaide areas) .have a greater chance of being obese and having diabetes and lung cancer and use health services more often.
The degree of inequality is disturbing. The most disadvantaged men and women in the region are, respectively, 59 per cent and 36 per cent more likely to be obese than their most advantaged counterparts. The most disadvantaged were 33 per cent more likely to report a mental health or behavioural problem and were 17 per cent more likely to have arthritis. The most disadvantaged men were nearly twice as likely to die prematurely, the most disadvantaged women 51 per cent more likely to die early.
And the most disadvantaged are 2.3 times more likely to attend hospital casualty departments, 2.4 times more likely to have consultations with specialists and 2.3 times more likely to be admitted to public hospitals.
Clearly, a greater emphasis on primary care is needed to lessen the use of hospital casualty departments and to address obesity.
Posted by Gary Sauer-Thompson at 9:14 PM | Comments (2) | TrackBack
December 5, 2005
Queensland health #2
The
The future of an ageing Australia is one of massive tax increases to pay for inadequate services. Hence Premier Beatties' view that the Australian health system will fall apart by 2015 and his call for a national health summit.
An editorial in todays Australian Financial Review takes up the issue. It says that:
Australia's health costs are spinning out of control....Last year Australia's total health bill topped $78.6 billion. Yet public hospitals are grinding to a standstill ....Something's wrong when when a system consumes 9.7 per cent of gross domestic product fails to deliver a reasonable standard of service. The Federal government knows it.....But more resources and skilled people won't solve all the problems...Most of the problems in health provision are about management of financial and human resources. Queues will shorten and services will improve if they are funded, paid for, and managed with clear lines of accountibility.
Very true. But hospitals are not the health system. There is the whole domain of primary health care outside the hospitals; a domain that functions to prevent illness and to reduce the flow of sick people into our hospitals.
Posted by Gary Sauer-Thompson at 3:55 PM | Comments (0) | TrackBack
December 1, 2005
Queensland health
The Davis Report into Dr Jayant Patel, the rogue surgeon whoss botched operations at Bundaberg Hospital resulted in at least 13 deaths, highlights the mess the state's health system is in. There is a culture of coverup in political, administrative and medical culture, chronic underfunding of the hospital system, and a lack of concern to keep the population healthy.
Inquiry commissioner Geoff Davies, QC, stated that the culture of secrecy involved:
"... involved a blatant exercise of secreting information from public gaze for no reason other than that the disclosure of the information might be embarrassing to government...This culture started at the top, with successive governments misusing the Freedom of Information Act to enable potentially embarrassing information to be concealed from the public. Unsurprisingly, Queensland Health adopted a similar approach, and because inadequate budgets meant that there would be inadequate health care, there was quite a lot to conceal. Again unsurprisingly, the same approach was adopted by administrators in public hospitals, and this, in turn, led to threats of retribution to those who saw it as their duty to complain about inadequate health care."
The health system is a mess yet Peter Beattie, the Queensland Premier, is calling for more funds, not ways to keep the population healthy even though obesity is looming on the horizon as a major health issue. Obesity is still ignored as an illness. Health and medical professions concentrate on treating its results---heart disease, diabetes, hypertension, gallstones, sleep apnoea, bowel cancer, etc. Yet obesity is a preventable disease through changes in diet and by becoming more physically active. It is spreventable because the main causes of obesity are sedentary lifestyles and high fat, energy dense diets.
The health promotion approach--giving out healthy lifestyle messages-- has failed whilst the weight loss medications is that theyŌĆÖre used as a way of avoiding getting exercise and eating less. ye te Premier never mentions health in terms of lifestyle modification.
Posted by Gary Sauer-Thompson at 7:16 AM | Comments (0) | TrackBack
Queensland health
The Davis Report into Dr Jayant Patel, the rogue surgeon whoss botched operations at Bundaberg Hospital resulted in at least 13 deaths, highlights the mess the state's health system is in. There is a culture of coverup in political, administrative and medical culture, chronic underfunding of the hospital system, and a lack of concern to keep the population healthy.
Inquiry commissioner Geoff Davies, QC, stated that the culture of secrecy involved:
"... involved a blatant exercise of secreting information from public gaze for no reason other than that the disclosure of the information might be embarrassing to government...This culture started at the top, with successive governments misusing the Freedom of Information Act to enable potentially embarrassing information to be concealed from the public. Unsurprisingly, Queensland Health adopted a similar approach, and because inadequate budgets meant that there would be inadequate health care, there was quite a lot to conceal. Again unsurprisingly, the same approach was adopted by administrators in public hospitals, and this, in turn, led to threats of retribution to those who saw it as their duty to complain about inadequate health care."
The health system is a mess yet Peter Beattie, the Queensland Premier, is calling for more funds, not ways to keep the population healthy even though obesity is looming on the horizon as a major health issue. Obesity is still ignored as an illness. Health and medical professions concentrate on treating its results---heart disease, diabetes, hypertension, gallstones, sleep apnoea, bowel cancer, etc. Yet obesity is a preventable disease through changes in diet and by becoming more physically active. It is spreventable because the main causes of obesity are sedentary lifestyles and high fat, energy dense diets.
The health promotion approach--giving out healthy lifestyle messages-- has failed whilst the weight loss medications is that theyŌĆÖre used as a way of avoiding getting exercise and eating less. ye te Premier never mentions health in terms of lifestyle modification.
Posted by Gary Sauer-Thompson at 7:16 AM | Comments (0) | TrackBack
November 15, 2005
where is the health policy?
I've been attending a health policy and services research conference in Canberra. It is strong on the services and low on the policy. The academics have little to say about policy ----addressing the problems they identify in relation to health care reform. They kinda back off and they aren't really willingly to cross the line over into the policy arena.
There was no presence from the policy think tanks eg., CIS. Nor was there a public presence from the senior federal bureaucrats or ministerial staffers who actually do policy. The conference is a platform to present the specialised work of Australian health academics with import from good quality policy people from the US and the UK.
The inference? There is a disconnect between academic research and public health policy despite the work done by Treasury and Productivity Commssion about rising health care costs and health workforce reform. Even when the need for a regulator for the health sector is discussed ---given the medical scandals (Camden, Campbelltown and Bundaberg) and the regulatory failure amongst managers and professional bodies has bought self-regulation into disrepute.
If the instruments of a health market and greater competition are going to be used to drive reforms in the health system, then there is a need for a strong regulator to prevent the anti-competitive behaviour of the medical profession out to protect its interests at the expense of consumers. What sort of regulator should that be? No answers were offered. That's too political.
Here's a suggesiton: why not the ACCC? Or why not a strong regulator for the health industry--along the lines of the British Health Care Commission?
Update: 16 November
Today's conference sessions indicated the bias and prejudice amongs the academic community to the policy world. The latter is a world of unreason, ignorance ,indifferent to knowledge and data, dot points, and pretty concerned with getting votes. This cartoon representation by the health economists from this mob was then contrasted with academic research world of reason, truth and enlightenment. The irony was that this duality and polemic was presented as the truth without any consideration being given to the work of the old Senate or the Productivity Commission in the formation of public policy.
The health economists are moving into health research in a big way--based on their ability to do economic modelling. The economic modelling is about economic or market relationships between individuals without any consideration being given to power relationships in the medical system. When this shortcoming in their assumptions is pointed out to them, and it is suggested that this means that their modelling would fail to capture both the medical dominance and gaze and the anti-competitive behaviour of the medical profession, they just shrug their shoulders and dismiss the criticisms of their assumptions with disdain.
Who cares is their response. They represent truth. The critics are ignorant of economics, prejudiced and biased.
My assessment of this conference? Our major or prominent research universities are self-absorbed institutions, compromised by their close relationship with government and corporations. They are given enough of the research to pie to be complacent, and they are coming close to being unwilling to deal with the fundamental moral and political questions posed by the failures of the health care system.
Posted by Gary Sauer-Thompson at 4:27 PM | Comments (0) | TrackBack
November 3, 2005
scarry narratives
We have so many scarry narratives these days, and our politics has internalised the culture of fear. Another scarry narrative is the one around bird flu because of its capacity to jump species.
That has happened, and the virus has transferred from one person to another. This transfer from person to person has been limited and it has stopped. It hasn't continued to move on.
So far.
What if? What if we are wartching a pandemic unfold in slow motion? Peter Martin offers an account in his A punter's guide to the pandemic
The government's response? The same as in the other scarry narratives: Trust me. Trust me. Trust me.
Posted by Gary Sauer-Thompson at 7:48 AM | Comments (1) | TrackBack
October 20, 2005
health: pressure points or system failure?
Well you can see the pressure points in the health care system. Here and here. Public hospitals and mental health.
The Queensland health system is widely seen as "unsustainable" without dramatic changes, and that would cost an estimated $1.5 billion a year to fix. Even though Canberra has reduced health funding to the states for years, Queensland have been under funding their mismanaged public hospital system for years.
Premier Beattie was on Radio National Breakfast this morning, and in the media throughout the day, doing his usual spin covering up the lack of inverstment in health; why patients will now make a contribution for minor elective surgery, adult dental health care, glasses and specialist outpatient services; and why it was no big deal to dump the basic principle behind Medicare--universal health care.
It did not occur to him, nor did anyone ask him, why adult dental health care or optical care (glasses) are being dealt with by public hospitals. Isn't that preventative medicine or primary health care that is treated in clinics outside public hospitals? Isn't Queensland meant to be the smart state?
The report into mental health Not For Service, was prepared by the Mental Health Council of Australia, the Mind and Brain Institute and the Human Rights and Equal Opportunity Commission, and it is based on data collected across the country from 2003 to 2005. It is littered with personal stories of loss and despair and describes how system and service failures resulted in worsening illness and, too often, death.
Immediately the states and commonwealth go at one another's throats to shift the blame. I'm with Commonwealth on this one. The drive for national mental health reform in Australia in the early 1990s (de-institutionalization) has hit a brick wall, largely because of the state's dismal record of funding reform (better community services that kept people out of hospital) and placing the emphasis on law and order. For instance, Tthe report dams SA:
Despite repeated inquiries and multiple government commitments, there has been little evidence of substantial mental health reform in South Australia. It remains the State with the greatest emphasis on institutional forms of care. While a great deal of community, media and professional criticism has been expressed about proposed changes to the mix of hospital and community care, there is also a clear desire for real reform. Reform will need to be backed by genuine resource investment as well as real leadership.
However, the Commonwealth's solution ---the Commonwwealth taking over mental health in order to provide enough psychiatric beds in public hospitals --is flawed, as it turns the clock back to institutions and away from the community.
Federalism is not the problem. Does it matter who delivers the mental health services? Couldn't the Commonwealth bypass the states and directly fund ngo's that deliver mental health services if the states don't lift their game. The indication is that they won't given the negative response by NSW Health Minister, John Hatzistergos: the reports methodology was questionable and its recommendations flawed. Yet in NSW, though money is spent on acute mental health facilities within hospitals, this is at the expense of community mental health centres which are being cut back.
Posted by Gary Sauer-Thompson at 8:13 PM | Comments (0) | TrackBack
October 6, 2005
health care reform: a suggestion
Ross Gitten's op. ed. in yesterday's Sydney Morning Herald is about health care reform and the Productivity's Commission position paper on the health workforce. It is unusual because there is little commentary on health care reform in the media. What we have is a health poltics based on newspaper headlines about huge hospital queues. not health policy.
Gittens starts his op. ed. on health policy by noting the significance of health care reform:
If you want to see the future, think health care. Report after report tells us the health industry's likely to be one of the fastest growing parts of the economy and the factor putting most upward pressure on the taxes we pay. Now we learn that health care's likely to be one of the areas of most pressing labour shortages.
Health care reform is big --it is much bigger than the much heralded waterfront reform of the 1990s. But you would not know that from the media.
Gittens grasps a key problem of health care as it is analysed by economists. He states that spending on health care will continue to rise as demand increases, and outruns supply of the services provided by the health care workforce. This disequlibrium will deepen because the shortages of the health workforce will get worse. Gittens says:
So, if we're almost certain the health system's present shortages are set to get a lot worse, what should we be doing?The obvious answer is spending a lot more money on extra training places...But it's equally obvious that such a response won't be adequate... merely throwing more money at problems quickly gets to be too demanding on the pockets of the taxpayers supplying the money. So the Productivity Commission's main message is that we should be doing a lot more to raise the efficiency with which people are trained and used in health care - which would, of course, raise their personal productivity.
What does efficiency and productivity mean?
Gittens addresses this by pointing to the direction in which health care reform needs to go: --that we ought to be investing a lot more of our effort on health promotion and preventive medicine. The health care focus needs to shift from acute illness and hospitals to good primary care. That shift is a big reform. Very big.
Will it happen?
Gittens grasps the central blockage to this pathway of reform: the patch protection by doctors and specialists. He gives a classic example:
Then there's the way doctors try to hog all the tasks (and the income that goes with them) - always in the name of preserving the quality of treatment and the safety of patients, naturally. Take the celebrated attempt to have properly trained "nurse practitioners" take over some of the more routine tasks performed by doctors. Doctors have resisted this all the way, and still are. From the initial investigation of the concept in the early 1990s, there are still only a handful of nurse practitioners in Australia.
There are plenty of other examples: the resistance to midwives, the GP's refusal to refer patients with muscloskeletal conditions to chiropractors, and the denigration of allied health care professionals by orthodox medicine. Efficiency means removing these blockages.
Gittens notes the way that the Medical Benefits Scheme reinforces "medical dominance ", as it is premised on doctors doing things that less trained (and less expensive) health professionals could do just as well:
Because most services provided by other health professionals and nurses are excluded from a Medicare rebate under the scheme, many patients prefer to have the service provided by a doctor. Doctors should be able to delegate routine tasks to other professionals - possibly working for the doctor - but, if they do, no one gets a rebate.
Thus we have the wasteful allocation of scarce resources. So you can see why Treasury and the Productivity Commission are interested in, and are driving, health care reform in the name of efficiency and productivity.
What Gittens does not address is the different pathways of primary health care. Not every allied health professional wants to be deskilled by working in a GP practice. Health care reform would recognize, and accept, that allied health care professionals can provide a different primary care pathway to that of the GP's. Gittens, by remaining too doctor focused, does not see the big consumer shift to a lifestyle or wellness conception of primary health care. It is this conception of primary health care that will lead to big productivity gains within the health workforce.
Posted by Gary Sauer-Thompson at 7:21 AM | Comments (25) | TrackBack
September 30, 2005
Questioning medical dominance
Do we have the beginings of health care reform in Australia, as opposed to the day to day political management of media headlines by the states in relation to to hospital queues and mental health? We saw some signs of this with federal Treasury's recent interest.
Treasury is obliged to do so because health spending is rising. Today's Australian Financial Review reports that the Australian Institute of Health and Welfare publication Health Expenditure Australia 2003-2004 states that health spending accounts for 9.7% of Australia's economy, that it is rising faster than both inflation and economic growth, and that households are bearing the brunt of rising health costs.
Yesterday the Productivity Commission released an issues paper on the health workforce. Entitled 'AustraliaŌĆÖs Health Workforce' it acknowledges a key problem, namely:
There are considerable pressures on AustraliaŌĆÖs health workforce ŌĆö as evidenced by shortages of supply in some professions, particularly (but not only) outside the major population centres, and a significant reliance on overseas trained professionals. In the future, ageing of the population will compound the impacts of other factors that will increase demand for health workforce services.
This supply shortage is well known in terms of primary health care, emergency and acute hospital services and specialist services. The Commission then opens up two ways to address this shortage:
Initiatives to boost the numbers of education and training places will be an important part of the response to both current shortages and increased future demand for health workers. But there is also scope and need to increase the productivity and effectiveness of the available health workforce and to reduce its maldistribution. Addressing a range of systemic impediments will enhance the capacity of the workforce to respond in an efficient and timely manner to the challenges of the future.
That puts an emphasis on increasing the productivity of health professionals as well maintaining high standards. The AMA mostly talks in terms of safety and standards and protecting doctors as gatekeepers of the health care system.
The Productivity Commission's economic approach to health care reform has implications for GPs, biomedicine and medical dominance because the continual propping up of GP's and medical specialists to ensure high health safety standards will not ensure a healthy population or wellness. The medical bodies have a lot of poiltical clout, and their big union, the AMA, consistently runs a safety fear campaign whenever their patch protection, cash flow, closed shop culture and status is criticised and challenged.
The Federal Government does recognize this. Tony Abbott, the Minister of Health and Ageing, is reported as saying:
The Government has no wish to diminish the role and the standing of the medical profession. But while respecting the knowledge, the commitment and place of the medical profession we obviously want to make full use of the whole of our health work force.
That means an increased role for allied health care professionals. The writing is on the wall in that it challenges the AMA's position that health care reform threatens standards and that only doctors can, and should, deliver health care. As they see it, they own Medicare. However, as yesterdays editorial in the Australian Financial Review pointed out, Australia has needed health care refrom for decades. The health system can be reformed without threatening standards.
What does this mean in terms of health care reform? Does it mean simply streamlining the system to ensure a cost-efficient health service? Not necessarily. One pathway of reform is for the state governments to allow hospitals to step in and coordinate the allocation and supply of all health care workers. Another pathway is suggested by Federal Treasury in the 2005 Winter issue of Economic Roundup. The relevant article is by Janine Murphy and it is entitled ">Health Promotion. Another reform pathway is to shift the focus away the medical institutions and their patch protection battles to the consumer. This would loosen up the medical market through competition to allow consumers to express their choice and sovereignty about the health they wanted.
Good public health policy should move into a reform mode to ensure the wellbeing of the Australian population. That means making sure that the neo-liberals do not succeed in increasing tax cuts by cutting back on health services to deal with the rising costs of health. It also means making sure that growth expenditure is addressed through health care reform to achieve population wellbeing and not cost cutting by razor gangs in the Department of Finance to keep the budget in surplus.
Maybe, just maybe, the pressures within the health care system have built up to a point where the Howard Government will accept the Productivity Commission's recommendations to increase the productivity of the health care workforce.
Posted by Gary Sauer-Thompson at 8:39 AM | Comments (0) | TrackBack
August 11, 2005
Tony Abbott on health reform
Health is one of those public policy issues that sits in the political background and then hits the media headlines with high costs, budget blowouts, long hospital queues, poor services, bad administration and death. Behind the media headlines the Howard Government has undertaken some useful reforms of the health system. Tony Abbott, the current Minister of Health and Ageing, describes these reforms this way:
"...the Howard Government has rescued the private health insurance system, lifting coverage from 30 per cent to 43 per cent of the population and taking pressure off the public system. The Government has introduced a new Medicare safety net, based on the fee charged, to protect people with high out-of-pocket costs who are not covered by private insurance. The Government has boosted bulk-billing from 66 per cent to 73 per cent of GP consultations; increased medical student numbers by 30 per cent; introduced much longer medical consultations for the chronically ill; and given allied health professionals access to Medicare for the first time."
It's a good description of what has happened. The Minister then says that the conservative principle is not "states' rights" but "if it ain't broke don't fix it" - or more of a concern with right outcomes than right theories. He rightly says that there are no panaceas for addressing the current flaws in the health system:
"..the trouble with reform talk is the underlying assumption that there is some comparatively straightforward change, usually a philosophical one, that, once implemented, will make the problem swiftly and painlessly disappear. Market-oriented reformers assume that price signals will solve all problems.Admirers of Britain's National Health Service think that planning and co-ordination are the universal remedy. There's much to be said for more price signals (even in health) as well as for good planning, but neither is a panacea if only because what's a solution to an economist is usually a problem to a consumer."
Alas, the minister then contradicts himself.
He reckons that:
The only big reform worth considering is giving one level of government, inevitably the federal government, responsibility for the entire health system. It won't resolve the eternal conundrum of how to provide better services while keeping costs down. It probably won't save the $2 billion a year predicted by some modellers but it will, at least, mean that there are clearer lines of responsibility and less incentives to make decisions on the basis of who pays rather than what's best.
However, he realizes that this kind of centralism, which deguts federalism, is not politically realistic. What is suprising is the Minister's lack of awareness about the way that he has dumped his conservative principles, and been seduced by big reform and sided with big theory. He has forgotten his Hayek and fallen to the fatal conceit of the socialists.
What is even more suprising is what the Minister does not say: that the importance of primary health care is to help reduce public hospital costs and the increasing costs of PBS. That approach to health care, with its diverse GP and wellness pathways, can give us right outcomes without worrying about right theories.
Posted by Gary Sauer-Thompson at 8:29 AM | Comments (2) | TrackBack
August 3, 2005
Queensland Health
There is something quite rotten inside the Queensland Health bureaucracy. With the Jayant Patel saga Queensland Health's most senior staff have pleaded ignorance over knowledge of his credentials and incompetence until the scandal erupted. No one is responsible for the evil.
The Dr Berg case, (Dr Vincent Berg was a psychiatry registrar at Townsville hospital with bogus credentials) has shown how a concerted effort to raise grave concerns with the then minister and her top bureaucrats was doomed to fail and was swept under the carpet.
By all accounts Queensland Health is still not fully co-operating with Mr Morris and his staff running the Commission of Inquiry.

Should not the finger also be pointed at the Beattie Government? Despite the media impression of the government as vigorous, dynamic, and getting things done, it looks increasingly incompetent.
Is it not the state government responsible for a dysfunctional and gridlocked health department? Has it not fostered a political culture in which public hospitals are chronically under funded and a bureaucracy that is more focused on balancing budgets and being a business rather than delivering better clinical outcomes?
Oh, where's the AMA in all of this?
Posted by Gary Sauer-Thompson at 12:00 PM | Comments (5) | TrackBack
July 28, 2005
Health: unions rule don't you know
One of the key problems in the Australian health system is the way doctors protect their turf through their union--the AMA. The AMA acts to make sure that doctors are the only gatekeepers to the public health system.
This restriction on trade is crucial because the health system is beginning to shift from a focus on treatment of acute disease to prevention of sickness.
The AMA blocks increased competition from nurses, allied health professionals, and pharmicists in the name of cutting corners, and second rate medicine, and finite budgets.
The problem is that through the AMA criticizes others for being anti- competitive--the pharmacists for trying to block the entry of the Woolworths in to their sector--they lobby against any extension of Medicare to other health workers. The AMA hides its standover union tactics of holding governments to ransom behind the aura of being concerned with better health care.
The pressure is building in the health care system with poor medical care, increasing costs of public health budgets, workforce shortages and closed training shops designed to limit supply.
The cracks will appear in the rural regions where the shortage of doctors means bad health outcomes. There are suggestions of an appraoch that would train a new type of rural health worker who could diagnose and prescribe certain drugs thereby circumventing doctors' traditional monopoly on prescription rights. The new rural health worker would be a doctor-nurse hybrid. This roll back of GP monopoly would require would involve a new training course.
Another way to tackle the GP gatekeeper approach to health care is to devise alternative pathways to preventive health care than the GP drugs approach. That approach can be developed by allied health professionals.
Posted by Gary Sauer-Thompson at 10:10 PM | Comments (0) | TrackBack
July 21, 2005
a little insight
Whilst on holidays and watching DVD's I've been dipping into the news here and there-- a quick grab on Radio National Breakfastin the morning; a fast look at the 7.30 Report in the evening; and a glance at the AFR and a scan of some online newspapers during the day.
It is hard to miss all the publicity about John Howard as the global statesman that puts Kim Beazley in the shade.
However, I did notice the way the Minister of Health, Tony Abbott, has lost his reforming zeal.
Indications are is that he is buckling under the pressure from the the big drug companies in relation to the government's generic drugs policy. It's been four concessions/exemptions from the Government's decision to pay 12.5% less for all medicines in a therapeutic group when the first generic drug entered that group.
The Treasurer's response was spot on:
"...we donŌĆÖt want to pay any more than we have to. So if there is a generic pill then we ought to encourage the use of the generic rather than a brand. The PBS is not run for the benefit of pharmaceutical companies. It is run for the benefit of the patients. We have now got a co-payment in there but we have got to be rigorous about testing the new medicines, bringing to market generic brand alternatives, making sure that we donŌĆÖt have unnecessary medications on that scheme."
That gives a little indication of the way health has become dependent on drugs rather than primary health care.
Posted by Gary Sauer-Thompson at 1:38 PM | Comments (2) | TrackBack
June 2, 2005
health reform
Health reform will be on the agenda of a stormy CoAG meeting this Friday along with infrastructure bottlenecks, industrial relations and skill shortages. We can expect the usual set piece stoush and outraged politics.
Health reform is needed as the national health system is creaking and groaning under the strain. As John Dwyer, chairman of the Australian Healthcare Reform Alliance, observes:
About the only consensus to be found among those grappling with the need for reform of Australia's healthcare system is that the status quo is intolerable....the existing costly dysfunction must be corrected...the problems are a byproduct of the wretched jurisdictional inefficiencies that make state and federal governments responsible for different sections of our healthcare system.
Basically, the feds are responsible for primary health care whilst the states provide us with hospitals. Will there be a confrontation on health reform at CoAG, or will there be a search for common ground?
Dwyer reckons that Australia has reached a crossroads:
"Down one path lies the continuance and strenghtening of a system dedicated to providing quality care in a timely manner to all Australians, based on need, not the ability to pay--we all share the burden. The other road leads to a two tiered system characterised by a "user pays" approach, while the government cares for the truely disadvantaged."
Health care reform has continually been placed in the too hard basket.
My bet is that it is likely the Howard Government's first step, now that it has control of the Senate, is to require those who can afford it to leave the public system and be treated privately. Everyone else would remain in the public health system.
Jeffry Braithwaite argues against a two tier health system on the grounds that a American-style health system delivers worse health outcomes than a public one.
Dwyer calls for a public debate in health reform four main areas: primary care,training of our our health professsionals, inefficencies associated with the jurisdictional divide,an an electronic national health record. It is good to see the reformers moving beyond an efficient federalism and public hospitals. We need soem working parties sorting this outto find a pathway forward.
However, we have yet to see a shift to wellness as opposed to treating disease.
Posted by Gary Sauer-Thompson at 1:40 PM | Comments (0) | TrackBack
May 25, 2005
Queensland medical crisis
The Queensland health system is in crisis. The suspected number of deaths at the hands of Dr. Jayant Patel (Dr Death) at Bundaberg Hospital is now estimated to be around 87 along with a further 20 cases of patients suffering complications.
Giving evidence at the commission of inquiry into the events surrounding Dr Patel's activities at the Bundaberg Hospital, Toni Hoffman, the nurse in charge of the hospital's intensive care unit, said:
"It came to a point when we discussed all of the things we'd done, all the people we'd been to and we just thought, 'What on earth can we do to stop this man?'.We'd taken to hiding patients, we'd taken to telling patients they should ask for a transfer, we were doing all sorts of things we shouldn't have been doing."
Toni Hoffman is a whistleblower nurse. It appears that the hospital administration sided with, and protected, Dr. Jayant Patel. Why did they do nothing to stop him? Aren't hospitals meant to be about saving people's lives not killing people? Why did hospital and health department management ignore the gross surgical incompetence of Dr Patel, when it was reported by staff?
The response by the Beattie Government to this medical malpractice crisis is an interesting one. It has decided to split the health department into two:--into a hospitals department and a department of primary care and health service integration. The aim is to break the traditional power bases in the state's health bureaucracy. About time this happened.
This provides the opportunity for the government to control the funding balance between health prevention and treatment. Everyone says that health prevention, or primary health care,is a good idea but it has little policy substance in Canberra. It will be interesting to see what Beattie does with it.Will health prevention continue to be the poor cousin to hospitals?
Posted by Gary Sauer-Thompson at 3:25 PM | Comments (1) | TrackBack
April 19, 2005
Treasury is running health policy
I flickered through the Sydney Morning Herald this morning in Canberra, as I don't generally see the print edition in Adelaide. I came across Louise Dodson's article about the fourth term agenda of the Howard Government. Dodson is a senior journalist at Fairfax and so she knows what's what in politics.
She makes two points that I found of interest. She says that the Federal Treasurer, Peter Costello, is:
"...increasingly behind most of the Government's fourth-term policy agenda. He was the first to publicly back increased skilled migration, he has been pushing for greater participation in the workforce by encouraging older people and those on welfare to work, he has raised the issue of infrastructure bottlenecks and he has been advocating productivity increases through industrial relations changes."
I concur. But it is broader than this kind of economic policy, as Treasury has also grabbed hold of health care policy and placed it under the sign of fiscal sustainability.
We can see this from the second point that Dodson makes. She says that this economically-driven policy agenda has its roots in:
the Treasury's inter-generational report three years ago warning of the impact of the ageing population. Since then Treasury's mantra for improving the economy has been population, participation and productivity.
That 2002-3 Report was Budget Paper (No.5).The core argument was that the federal government "will need to make policy adjustments to maintain a sustainable fiscal position over the next four decades."
Dodson sees the population, participation and productivity drivers, which are the levers the Report says will help to reduce future budget pressure. Suprisingly, Dodson misses Treasury's emphasis on Australia's steadily aging population placing significant pressure on Commonwealth finances; and that technological advances in health care, plus community expectations of accessing the latest health treatments, would place increasing demands on taxpayer funds.
Dodson misses health stuff entirely. She is more focused on Costello's leadership challenge.
The detail of this skeletal policy framework of health care as a financial burden weighing down on younger generations is being sketched in by the Productivity Commission Reports. The core of
Treasury's Intergenerational Report is that the budget pressure from health care can be alleviated or eased by the effects of increases in population, participation and productivity. These drivers will help to grow the economy.
Had Dodson actually read the Intergenerational Report closely (Part IV, p.57), then she would have seen that Treasury's projections indicate that it is health and aged care costs that are going to blow the federal budget big time. It will be increasingly larger deficits from 2014 onwards, due to costs outrunning revenue. Disaster beckons.
Now Treasury's goal is to maintain an efficient and effective medical health system, complimented by widespread participation in private health insurance.Treasury is different from the Department of Finance run by bean counters, as it says that its aim is to manage economic policy to improve the wellbeing of Australians in a way that can be sustained over time.
However, wellbeing as the end of economic policy can only be achieved within the limits of ensuring that future generations of taxpayers do not face unmanageable bills for government services to the current generation. And those bills will become unmanageable after 2015. So we have to do something now by way of making cost savings to the health budget. This is being economically responsible. That is the new policy mantra.
I guess that Dodson is good on politics (leadership) and poor on policy.
Posted by Gary Sauer-Thompson at 10:42 AM | Comments (0) | TrackBack
April 16, 2005
Medicare rorting
The fallout from the Howard Government's Medicare safety backlip continues about commitments that were:

The anger and criticism is justified because the Howard Government knew about the cost of the safety net, and that it would be extensively used by the middle class going to see the specialist. They were prepared to wear the cost and they trusted the specialists to do the right thing.
I mentioned here that all the fuss being made about economic responsiblity, economcially sustainable health system, the broken promises, the lack of political credibility and the bucket loads of deceit and spin obscures the real issue whichis what is being ignored: the open rorting of Medicare by the specialists.
Well The Australian carries a report of the rorting by Adam Cresswell. Cresswell says that a medical specialist has accused his fellow specialists of fuelling the safety net blowout by charging hundreds and even thousands of dollars extra to the scheme - a direct challenge to the Government's claims that medical bills are not rising.
In a rare example of a doctor breaking ranks, the specialist said he knew of one case in which a doctor planning a patient's breast reconstruction surgery had charged $5000 for a preliminary consultation that was normally bulk-billed.The operation itself, which normally cost $5000, was then peformed for just $10 - a reversal of charging practice that ensured the vast bulk of the fee came under the safety net scheme. Because the safety net covers out-of-hospital costs but not in-hospital costs such as operations, the arrangement meant the patient could have recouped up to 80per cent of her out-of-pocket charges from the safety net.
Rorting is common practice, not an isolated example, and its existence is well known in policy circles. It often takes the form of increasing the (AMA-recommended) fee for a consultation of $130, to multiples of that ($500) as a way of transferring the in-hospital gaps on to the safety net.
This corruption highlights the flaw in current health policy that is not being addressed.
A lot of commentary repeats the Treasury line that:
"...the overriding aim of health policy should be to control demand - and its impact on the price of services. How else are governments to have any hope of managing soaring costs driven by escalating patient expectations?"
Given this kind of economic reasoning what is suprising is the silence of the Howard Government, the AMA and the ALP about this rorting, even though the Health Insurance Commission, which administers Medicare, has issued warnings to some specialists about their obsene behaviour.
If you were serious about containing costs, then you would seek to remove the rorting of crony capitalism in which a trade union has captured the Canberra Health bureaucracy and runs health policy. So I'll repeat my charge.
Both the Howard Government and the ALP lack the political courage to take on the AMA and clip its trade union wings.
Posted by Gary Sauer-Thompson at 12:04 PM | Comments (0) | TrackBack
April 15, 2005
public health & Treasury's hand
The health 'crisis' is usually represented as being one of rapidly rising spending on health care generally, and not just the public part of health care currently paid for by taxpayers. Health costs are escalating. Something has to be done.

Rising health care spending is due to both medical price inflation (eg., specialists such as radiologists and obstetricians) and the increase in the range of things that medicine can do with better technology.
The news today is that the Howard Government lifting the Medicare threshold for out-of-pocket medical expenses incurred out of the hospital. Families, pensioners and health card holders will now have to spend $500, up from $300, before the government picks up 80 per cent of the tab.For others the threshold will be lifted to at least $1,000, up from $700. The reason is a budget blowout.
That is the hand of Treasury. And the ALP follows the Treasury line by saying it is unsustainable and the Howard Government always knew it to be so.
What is being ignored is the failure by Tony Abbott to address the rising costs due to the medical price inflation caused by specialists increasing their fees. These price increases need to be capped and the rorts stopped. As there is no health regulator for the private health industry the market rules. What should be addressed is the lack of courage in tackling the AMA union.
The AMA is silent on this rorting. Sure it condemns the increases in the safety net threshold in the name of good medicine. But it protects its own by saying nothing at all about obstetricians changing their billing practices so that inhospital maternity costs not covered by Medicare are restructured as outpatient consultation fees.
And the senior journalists in the corporate media? How are they holding the Howard Government accountable? Louise Dodson in The Sydney Morning Herald merely reports the issue. Michelle Grattin in The Age concentrates on the broken promises and says nothing about tackling the specialists.
The Australian's editorial touches the issue then shies away to follow the Treasury line:
"The Government's decision can be criticised by doctors who assume the health of their bank balances is an excellent indicator of national wellbeing. And arguments it will hurt people who make most use of the health system are incontestable. But as it stands, the costs of the safety net cannot be contained, and this may not be the last change we see in the life of the Government. Mr Howard mistook throwing money at problems for a health policy in the last election campaign. All taxpayers, not just people who benefit from the safety net, are now paying the price of his profligacy."
Few are willing to take on the specialists. Not even the health economists from Australia Institute (Richard Deniss) or the Monash University Centre for Health Economics (Jeff Richardson). Only the Doctors Reform Society is willing to call a rort a rort.
Posted by Gary Sauer-Thompson at 12:56 PM | Comments (0) | TrackBack
April 13, 2005
Productivity Commision & health care reform
Health care reform in Australia often centres around our public hospitals. The story that is told is one of patients waiting longer for elective surgery, despite ever more money being poured into public hospitals by the federal and state governments.
In some states patients are waiting months longer for many common surgical procedures in 2004 than they did in 2002. Our public hospitals are under unprecedented pressure to meet budgets by cutting bed numbers and limiting access to operating theatres. In market terms the demand for medical treatment exceeds the number of doctors, nurses and hospital beds available.
One obvious solution is to shift the hospital-centric focus on the care of people who are ill and in hospital, and spend more on public health schemes that are designed to prevent illnesses. Receiving earlier primary care treatment by a GP or an allied health professional would keep many patients out of hospital.
Australia has a high level of hospitalisation because our level of primary care is fragmented, inadequate and too doctor-centric.
Into this debate steps the Productivity Commission's Economic Impacts of an Aging Australia. that had been commissioned by the Federal Treasurer. Addressing the issues before the baby boomers become old and sick provides us with an opportunity to think ouside the tight health, hospital, doctor nexus. The Report's economics of ageing paints a picture of rising health costs over the next 20 years that would have to be covered either by massive increases in taxes or containing spending and expanding the economy.
The Productivity Commission argues that keeping people over 65 in the workforce, reducing government spending on pensions, and removing remaining incentives for early retirement in the superannuation system could help governments meet the financial burden of an ageing population.
A lot of the response has been on expanding the economy by saying that the key is participation in work for the over-55 jobless. It's more work less play. Treasury, as you would expect, is talking about cost-effective health care provision meaning containing spending through Australians shouldering a bigger share of their own health care costs.
The federal Treasurer is talking about welfare-to work reforms that will form the centre of the May Budget.He means to shift thousands of people from welfare to work. His justification is that Australia will need to lift workforce participation rates to avoid a massive budget blow-out and tax burden.
The Australian Financial Review says the key is increased productivity, meaning getting more out of the diminishing workforce and making it more flexible. Then it goes on about reforming federal state relations to avoid duplication, rural producers paying market price for water, containing Telstra's vast monopoly etc etc; little of which has anything to do with health. It uses the issue to push its own reform barrow.
Hardly anybody is talking about reducing future health costs through preventive medicine that would keep an ageing population healthy, and so out of our public hospitals and aged care facilities.
Interesting silence that, don't you think. All the chatter is about short term politics. It commands attention for a while then dies down. The long term policy concerns are not addressed. Treasury's representation of the health care crisis is just accepted.
Posted by Gary Sauer-Thompson at 1:09 PM | Comments (3) | TrackBack
April 8, 2005
health, federalism, politics
Despite the irony it looks real bad:

Leahy
But it is not just Queensland. It is all the states in our federation. They are the ones who manage our large public hospitals. State governments have been given their public hospitals limited budgets and told to make do with less. This has meant rationing their services through ever growing lists and queues.
Now the states have been partly to blame for the chronic hospital waiting lists, (along with poor school standards, infrastructure lagging behind development, and broken promises on taxation). Their style of management during the 1980s and 1990s has been a form of economic management based on budget surpluses designed to preserve, or regain, their credit ratings instead of providing government services to reasonable standards.
The states have not been very smart on the politics of this. They've tried to deflect their responsibility by saying that the problem is Canberra, as it has cut back funding on the necessary funding.The states are not smart because they've being saying this whilst GST revenue has been rolling into their Treasury coffers. Being Labor states they continued to denounce the GST as a bad tax, even though it is growth tax that will give the states the financial independence they always wanted. It smacked of opportunism.
What the ALP state governments were doing was trying to disguise the way they had allowed themselves to be prisoners of Treasury group-think; and letting their neo-liberal Treasurys run human services in the name of sound finance or disciplined fiscal policy.
So the finger should be pointed squarely at the states as they really do need to lift their game. But the responsibility finger should not be just at the states.
The economic's profession is also partly responsible as they have advocated a particular economic mode of governance.
Their neo-liberal politics is about rolling back the welfare state, and they have said that good (rational) economics is to run budget surpluses based on cutting costs and reducing government services. The mentality behind this is that it is good that people suffer, as they will then appreciate that services cannot be provided free, and that they ought to pay for them through the market.
One consequence of this mode of governance by the states is the current commonwealth talk about a fundamental overhaul of the public health system; one that would bypass the states and fund regional authorities to oversee the provision of medical services and care. This basically means an increasing centralism with the commonwealth avoiding any dealings with the independnent states. Under this centralizing tendency the states will be increasingly sidelined, reduced to service deliverers, and given little role to play in national policy making. For more see Ken Parish's excellent post over at Troppo Armadillo.
It is an attack on federalism as it is an attempt to do away with division of powers in a federal polity. Power is going to the commonwealth's head.
Posted by Gary Sauer-Thompson at 11:14 AM | Comments (0) | TrackBack
March 30, 2005
Cancer: treatment pathways
Our general medical health care system is faced with ever-increasing incidence of cancer. The standard treatment is based on expensive, radiation and/or toxic remedies having serious side-effects, and severely impairing the quality of life.
In the previous post on cancer I suggested that we should avoid the current situation of either orthodox biomedicine or alternative treatment. Rather than this mutually exclusive approach we need a middle pathway in which the rigorous approach of an evidence-based medicine is used to assesse and evaluate the different treatment pathways to see how effective they are, and what side effects they have.
I then added that this basic information should be publicly available. If there is a politics of cancer then it should focus on the public's rights to know about the different treatment pathways, the different treatments, their effectiveness and their negative effects.

My reason for this taking this position is that a number of so called alternative treatments are really complimentary ones. The psycho-social approaches, for instance, help patients deal with the stress of going from being a healthy person to cancer patient for the rest of their life. The need for stress management is now widely accepted because it compliments the bio-medical model's lack of nurturing and lack of care. The bio-medical model does not deal with the life of a person, since it deals only with the bodily system or the organ.
What is not readily accepted by the biomedical cancer institution is the use of dietary treatments including the use of vitamins, mineral and herbs to help the body recover from the toxic effects of conventional radiation and chemotherapy treatments. The usual reason given for the widespread no is that these treatments have the potential to pose a risk to the patients's physical well-being by interfering with the effectiveness of the drugs involved in conventional treatment.
The quick response is: 'well, what does the research on this say'? Shouldn't we looking for the best treatment package to ensure the patient's wellbeing?
We know the answer in Australia. There is no research being done. Why? Because there is no funding? Why is there no funding? At this point the excuses run out and the appeal to evidence-based medicine is quietly put to one side and an ethical principle is pulled out. It is said that we should avoid those treatments that harm the patient.
Well, what about treatments such as radiation and chemotherapy? Do not these harm the patient? Why do we not avoid those?
SO what is the solution? It is simple.
There ought to be a publicly funded national centre to:
# co-ordinate and enhance research as it relates the prevention, diagnosis and treatment of cancer, cancer-related symptons ad side-effects of conventional cancer treatment;
# help identify promising non-conventional treatments for further research
# explore non-conventional treatments in the context of evidence-based medicine.
Such institutes exist in the US. Why not Australia? Why is there not similar institutional mechanisms to fund research into complimentary treatments in Australia?
What does appears to be off the radar is immunotherapy as a treatment pathway that uses uses certain parts of the immune system to fight cancer. We understand that our immune system is effective in combating infectious diseases caused by such invading agents such as bacteria and viruses. So why cannot the body's immune system play a central role in protecting the body against cancer, in combating cancer that has already developed, and in slowing down the growth and spread of tumors?
Does not the immune system recognize and destroy even large quantities of established tumor? Can we not treat malignant diseases either with immune cells or immune-active agents that are genetically or chemically modified to optimize their cancer-fighting properties?
Posted by Gary Sauer-Thompson at 12:03 PM | Comments (0) | TrackBack
March 23, 2005
Cancer Inquiry#3: some what ifs
I've been meaning to pick up on the previous posts on the newly formed Senate inquiry into cancer here and here. From what I understand submissions are currently being received by the Senate Community Affairs Committee. The first public submissions will be in Perth next week.
What I have noticed from reading some the public literature is how much the treatment of cancer operates within, and presupposes, the particular scientific paradigm of biomedicine. This relies on an essentially mechanical understanding of causation in which repairing a body is analogous to fixing a machine. Each disease has a specific cause that can be discovered by medical research.
This biomedical model or paradigm assumes that the cancer as the tumour is the disease; and not a sympton of a more systematic disease in the body.It holds that the tumour as disease starts locally, then slowly spreads through our body. Consequently, the treatment addresses the turmour by cutting it out (surgery); killing it or shrinking it (radiotherapy) or by poisoning it(chemotherapy). The aim is to eliminate the disease as tumour and achieve a cure.

The biomedical model provides a clearly articulated scientific framework for understanding the disease process and mechanisms of remedy, and it excels at treating infectious diseases and acute or traumatic injuries.
Mechanism (ie., the "body as machine" metaphor) and reductionism (ie., the reduction of illness to a set of physical symptoms) dominate biomedicine. Disease is seen as an outside invader that atacks a particular part of the body; treatment repels the invader. Thus, some cancers are known as "malignant" tumors; chemotherapy aims to "attack," "fight," or "beat" the cancer. The metaphor of fighting and wining the war on cancer justifies the toxic side effects of some of the treatments.
What if our health deteriorate to near death from the war? What if cancer is not just the tumour? What if cancer is a chronic, multifaceted illness having multiple causes amenable and multiple therapeutic interventions? What if we are not winning the war against cancer? What if the number of Australians getting cancer each year has risen over recent decades, while our ability to treat and cure most common cancers has remained virtually unchanged? Should we talking in terms of "cure" rather than recovery?
Should we not be moving treatment towards non-toxic drugs that can tell the difference between healthy cells and cancer cells and so avoid the situation of chemotherapy drugs destroying all cells? Why not starve the tumour but fed the body so that the body environment is less favorable for tumour growth? Why not have treatments that rebuild our body and its immune system?
An alternative model, a healing paradigm, understands the tumour to be a symptom of an underlying disease that causes the symptons. So the tumour symptoms spread throughout the most suspectible body tissue. This approach places an emphasis on boosting the body's immune system and on some aspects of psychotherapy because human beings are not just physiological mechanisms. We have social and emotional bodies that interact with the environment.
What is needed in this situation is not an either or: it is a rigorous approach of an evidence based medicine to assess and evaluate the different treatments, to see how effective they are and what side effects they have. That basic information should be publicly available. If there is a politics of cancer then it should focus on the public's rights to know.
Posted by Gary Sauer-Thompson at 3:58 PM | Comments (2) | TrackBack
March 5, 2005
Health care-American Style
The fear is that Australia's health system will become increasingly privatised and more like the American model:
We are already on a pathway of creating cost inflation and greater inequity in health care. There is a lot of rhetoric to ensure that this pathway is made politically acceptable.
In Australia we have to subsidize the private health industry.It is a classic example of an industry that offers a poor product and depends on corporate welfare.
The justification? People do not appreciate what is offered unless they pay for it.So say the neo-liberal policy makers and politicians.
Of course, what is forgotten is that we citizens have already paid for a public health system through our taxes.
Posted by Gary Sauer-Thompson at 11:44 PM | Comments (1) | TrackBack
February 21, 2005
Health reform: doctors rule
I see that The Australian is running its Sustaining Prosperity Conference again in association with the Melbourne Institute. Health reform is the issue today and it is not just about tinkering with the federal/state adminstrative machinery.
These remarks by Mary Anne O'Loughlin are to the point on health reform in Australia:
We are constantly told of the high and increasing expenditure on healthcare. But the fact is too many health resources are used to provide services to people with diseases and conditions that are known to be preventable.
The implication is that more resources should be devoted to prevent people from becoming sick in the first place. That makes sense doesn't it. It is better public policy to help keep people from getting sick than treating them in hospital when they are sick. Cancer caused by smoking is a good example of this approach.
Mary Anne points out that:
Reform is needed, but the debate has focused more on waiting lists for elective surgery than preventing the need for admissions in the first place. Most of the ill health, disability and premature death in Australia today arise from chronic diseases, such as cardiovascular disease, cancers, diabetes and asthma. A large proportion of this is preventable.
Alas that approach to public health is not happening. Why?
Mary Anne O'Loughlin is quite clear on this. She says:
In Australia, the debate about healthcare reform is overly concerned with how to get more people into hospital more quickly. At the federal election last year, the centrepieces of both the Coalition and Labor health policies targeted access to hospitals: the Coalition through an extension to its private health insurance rebate; and Labor through its Medicare Gold policy...
The emphasis is hospitals, not on primary health care that prevents people from becoming sick and ending up in hospital.
And, we can add, on primary health care the focus is on doctors as gatekeepers to the health system and not on allied health professionals.
That heavy hospital/doctor emphasis is the key to health reform in Australia. The lock is the trade union politics that keep the doctors running the health system.
Posted by Gary Sauer-Thompson at 3:21 PM | Comments (0) | TrackBack
February 16, 2005
cancer: cures and healing
This is a more philosophical post than is normal on the public opinion weblog. But it is about cancer and the Senate cancer inquiry initiated by Senator Peter Cook.
I've found the book online that Senator Cook mentioned was important to him in helping deal with his cancer, and which motivated his concern to set up a Senate Inquiry into evaluating different cancer treatments. It is Michael Lerner's 'Choices In Healing: Integrating The Best of Conventional and Complementary Approaches to Cancer'.
I notice that Lerner has also made the connection between health and the environment, in particular the way
...people are troubled by scientific evidence that manmade chemicals, the depletion of the ozone layer, climate change, and the new infectious disease agents emerging from habitat destruction may threaten their health and the health of those they care about.
After reading the Preface, Introduction and the first two chapters of Choices In Healing I realized that here is the modern verison of the classical conception of a therapeutic, ethical philosophy as a way of life, or an art of living well.
This conception of philosophy is motivated by a therapeutic concern to remove those poisonous beliefs and values that make our way of life sick. The task is just like the medical doctor, namely, to identify what makes us sick, offer a diagnosis and suggest a remedy that will cure the sickness. The basic argument is that many of the ills we suffer from are due to mistaken beliefs about what is truly good, by which is meant a flourishing life well lived. The diagnosis is that we have invested our hope in the wrong things, or at least invested it in the wrong way. Our capacity to flourish and be happy (to attain eudaimonia) is dependent upon our own characters, how we dispose ourselves to ourselves, to others, and to events generally. The aim of this conception of ethical philosophy is to help us to live flourishing lives by dealing with those ideas, values, beliefs and practices that help to make us sick.
How does Michael Lerner reconnect with this classical conception of philosophy that has been all but forgotten?
He does so with his distinction between curing and healing, which he says lies at the heart of all genuinely patient-centered approaches to cancer treatment and care.He says:
...a cure is a successful medical treatment. In other words, a cure is a treatment that removes all evidence of the disease and allows the person who previously had cancer to live as long as he would have lived without cancer. A cure is what the physician hopes to bring to the patient. Curing is what the doctors hope to do...
On the other hand, healing is an inner process through which a person becomes whole:
Healing can take place at the physical level, as when a wound or broken bone heals. It can take place at an emotional level, as when we recover from terrible childhood traumas or from a death or a divorce. It can take place at a mental level, as when we learn to reframe or restructure destructive ideas about ourselves and the world that we carried in the past.
Cure and healing are intertwined.
Lerner says that the starting point for informed choice in both mainstream and complementary cancer therapies is the patient's recognition that s/he can play a crucial role in the fight for his life through the healing process. It is the healing process that enables each of us to reach beyond choices about therapy to choices about how we intend to live each day for the rest of our lives. Healing is Lerner's name for the classical conception of philsophy as a way of life or the art of living well.
If we re-describe the cure/healing distinction into public health policy terms we have the discourses of biomedicine and allied health (which Lerner calls biopsychosocial medicine).The biomedical discourse is about physical processes of disease, the relief of pain and physiological process of curing. The allied health discourse is about the human experience of disease (illness), pain (suffering) and the human experience of healing.
Biomedicine's knowedge/power (science plus the biomedical-industrial complex) works to separate itself from allied health and biopsychosocial medicine. The knowledge-power of biomedicine understands the physician-scientist to be a technician who offer the patient his technical/expert skills, and deploys the mind body duality to stay out of what they describe as psychological and spiritual issues. The medical gaze of biomedicine sees allied health as inferior practice rather than a complimentary one.
An interview with Michael Lerner.
Posted by Gary Sauer-Thompson at 8:17 AM | Comments (0) | TrackBack
February 13, 2005
Cancer, politics, ecology
On Thursday when I was in Canberra I noticed that the Senate had agreed to set up an inquiry into cancer treatment in Australia by the Community Affairs References Committee, which will look at the various options for cancer treatment in Australia. This provides a venue for authentic deliberation within the formal institutions of the state.

Hopefully, the inquiry will also look into the causes of this disease, since the why question is a very important one. Information about the causes of cancer in Australia should be publicly available, given that around one-half of all the world's cancers occur among people living in industrialized countries, even though such people are only one-fifth of the world's population. We need a three-part inquiry: a looking into past exposures, a reassessing of the present situation including the various treatment options and imagining an alternative future.
Hopefully, the Senate inquiry will explore the first two parts and begin to tackle 'the talk about cancer' in terms of social medicine: as a medical discourse and the oppositional allied health ones; instead of an aggregation of individual public opinions in the public sphere outside the institutions of the state.
I first become aware of the importance of the why question from reading Sandra Steingraber's book Living Downstream: An Ecologist Looks at Cancer and the Environment several years ago. It's a very good book. Do read it, if you can, as it questions the rigid assumptions of the cancer establishment in a way that makes sense to those living downstream of the Murray-Darling River system, as I do.
We should thank Senator Peter Cook for his efforts to establish the Senate inquiry. As far as I could see this event was not reported in the media. So the many kinds of silences that surround cancer issues-personal and political, individual and collective-continues. However, Alan Ramsay in the Sydney Morning Herald picks up what Senator Cook had to say, and provides the background.
It really is about time this inquiry happened.
Cancer is a big killer in Australia. One in three Australian men and one in four Australian women will develop cancer before the age of 75.Over a quarter of all deaths each year in Australia are due to cancer. Though our current knowledge suggests that least one third of all cancers are preventable (eg., those caused by smoking and damaging levels of sun exposure) there is is a growing awareness that many cancers are caused by the pollutants, pesticides and toxic chemicals in our environment.
The causal role of environmental pollutants (PCBs, DDT, and DDE (a DDT breakdown product) is rarely mentioned in Australia, even though these organochlorine pesticides (products of the chemical industry) are increasingly in our bodies.
Maybe the Senate inquiry will provide a political space for the many stories to be told; will enable Australians to become better informed about the link between toxic chemicals, body burdens and cancer; and give them the information they need to start making some noise.So many Australians are being amputated, irradiated and dosed with chemotherapy. They--and they are unknowns--expire privately in hospitals and hospices and are buried quietly.
In his statement Senator Cook said that the inquiry into services available to cancer patients and into treatment options, including less conventional therapies, is aimed at practical help for the one in four Australian families hit by cancer that causes enormous peronal suffering. He adds:
Specialist health care [here] is among the best in the world. But there is a bewildering number of adjuvant therapies and less conventional approaches which offer varying degrees of help, some overstated, some not, which can be significant if not decisive. Doctors tend to stick with proven treatments, whereas patients are often desperately looking for the most promising options to improve their odds. This dichotomy and the dismissive attitude conventional medicine often exhibits towards less conventional treatments can leave patients worried and confused.
It is about time this door was opened up on the medical cancer establishment's governance of cancer, because cancer cells are mostly created, not born. Families share environments as well as chromosomes, as our genes work in communion with substances streaming in from the larger, ecological world. Hence the modern biomedical trend to focus on the genetic causes of cancer, is a sidepath. We should be looking at the toxic world we live in.
Senator Cook then addresses the politics of cancer treatment:
The health debate is understandably dominated by doctors, heath-care professionals, health bureaucrats and academics, all with the apparent needs of the patient at heart but with transparent self-interests of their own. If this inquiry can stand in the shoes of patients and unambiguously take their point of view, it will be a breath of fresh air.
Most of the medical research by the medical establishment is basic scientific research at the cellular and molecular levels, which is done in an effort to detect, diagnose, and treat disease. Apart from smoking and sun screen little effort is being devoted to prevention by reducing our exposures to cancer-causing chemicals in our air,water, and food.
It is sad to report but the powerful cancer medical establishment continues to deny the importance of environmental factors and that view continues to be perpetuated. It is stated that only two percent of cancer deaths are due to environmental causes. But how many Australians is that? Is it more than more than the number of women who die each year from hereditary breast cancer? Is it more than the number of nonsmokers estimated to die each year of lung cancer caused by passive exposure to secondhand smoke in pubs, bars and resturants?
Posted by Gary Sauer-Thompson at 9:22 AM | Comments (4) | TrackBack
February 10, 2005
mental health
It is not often I agree with Miranda Devine but I do this time. Her op. ed on mental health is bang on target. She hopes that the Cornelia Rau case forces the longstanding disaster of our treatment of the mentally ill to the top of the national political-media agenda. So do I.
Devine says:
But far from being an anomaly, [Cornelia Rau's] tragic case is the norm for many psychiatric patients. They lurch from one psychotic episode to another, and wind up in the jail system, which has evolved over the past decade or so into a de facto mental institution without adequate treatment facilities.
Devine highlights two problems in the treatment of the mentally ill. The first is that:
A national shortage of acute-care psychiatric beds means psychiatrists in public hospitals have had to "raise the bar" on just how ill a person needs to be before being admitted.
The other problem is that:
...there is no systematic provision of community-based, hostel-style accommodation, offering various types of support for the mentally ill as their illness fluctuates. For instance, attached to Cumberland Hospital in the 1980s, says Barclay, were "villa wards", a type of hostel with 20 patients, each in their own room, with a central kitchen where patients could be served or prepare their own meals, and a clinic where a nurse supervised medication and kept an eye on them.
These problems indicate that primary mental health care should be a key policy priority as it the ssytem is close to collapse and urgently in need to revitalisation and additional resources.
Most Australians who seek help mental health problems usually see their GP first. However, Australia has only begun to take primary mental health care seriously and only begun to link it to allied health and mental health experts.
There ought to be a Senate inquiry on this issue set up before 30th June. Will the ALP have the political courage to take up the motion of the Australian Democrats to set up an inquiry?
Posted by Gary Sauer-Thompson at 9:35 AM | Comments (6) | TrackBack
August 26, 2004
Health: ALP collapses?
The Howard Government's approach to health is not quite as bad as this:

Moir
Extending the increase in the bulkbilling rates to the suburbs in the major cities was not bribery. It was good policy, given the low rates of bulkbilling there. That move had placed out of bounds in the MedicarePlus negotations between Tony Abbott and the 4 cross bench senators earlier this year. The extension was needed. It is to be applauded.
What was missing from MedicarePlus was a shift to funding quality health care based on 15 minute appointments, rather than a 6 minute tick and flick bulkbilled health care.
Abbott's recent extensions to the private health insurance rebate (from 30 per cent to 35 per cent for those aged 65 to 69 and 40 per cent for people over 70) Abbott has managed to box the ALP into accepting the private health insurance rebate. The ALP now lacks the courage of its convictions to stand firm on its previous policy of abolishing the rebate to defend a universal Medicare.
All that the ALP currently says is that it will not let the recent Band-Aid changes through the Senate. My bet is the ALP will blow all hot and passionate before the Senate cameras about the rebate whilst quietly letting Abbott's changes through.
Does not that low target strategy tacitly endorse a two-tier system that entrenches distinctions between those with private insurance and those without? Does that not mean the ALP is supporting the present size of the private sector with huge outlays of taxpayer money? Where is the equity there?
So it goes along with the myth fostered by the Howard Government that the 30 per cent rebate on private health insurance offered to the middle class to encourage them take out private health insurance are in fact designed to strengthen Medicare. The reality is that the rebate is funded by
Is the ALP planning to allow people to flow back to Medicare as the cost of private insurance increases faster than inflation when it regains the Treasury benches?
What the politics of health means at the moment is that Howard is able to fight on the ALP's own ground. The ALP's historic advantage of being trusted by Australians to ensure better health outcomes for them has been squared.
Posted by Gary Sauer-Thompson at 9:57 AM | Comments (0) | TrackBack
July 11, 2004
Medicare: a problem
This account by Max Walsh of MedicarePlus is about right. He says that Tony Abbott was parachuted into the health portfolio to salvage what was fast becoming a political black hole for the government.
Abbott succeeded in plugging the blackhole. Health is not a big issue in the election campaign.The ALP has lost is historic advantage. However, there is a cost for this political fix. Walsh highlights the key problem:
"The central feature of the safety net is that it does away with the concept of a scheduled fee as a means of capping the exposure of the tax coffers to the demands of the medical profession....Abbott rejects that the medical profession will increase fees, saying it is not out to rip off people. But he has changed the rules of the marketplace .... In fact, Abbott has given the green light to obstetricians and surgeons to change their way of billing patients by shifting the major element of their fees onto surgery consultations rather than hospital fees. While this could mean lower costs to patients, it is much more likely this will be shared between doctor and patient."
Was Abbott's refusal to cap specialist fees a way of keeping the AMA onside, whilst the Medicare doors were opened to the allied health professsionals?
Is the ALP quietly dumping its universality principle in the name of economic responsibility? What does that mean for health reforms?
It has accepted the Howard Government's principle of a mix of public coverage bolstered by heavily subsidised private insurance. Labor is committed to maintaining the 30 per cent rebate for private health insurance. It has agreed to the Howard Government's changes to the Pharmaceutical Benefits Scheme.
What does universality mean when all this is in place?
Posted by Gary Sauer-Thompson at 10:42 PM | Comments (0) | TrackBack
April 23, 2004
Health: reform on the way?
A CoAG ministeral meeting about health care took place in Canberra today. Mark Metherell at the Sydney Morning Herald has some comments. He says that an alliance of 22 national health groups will challenge the ministers to investigate proposals for a single funding system and report back by July, only months before the federal election. Some have been advocating such ideas for many a long time.
The Australian Health Reform Alliance have proposed the creation of a Central Australian Health Commission to end blame-shifting between States and Canberra. The new body would hold Australia's health budgets in a single account and be responsible for running hospitals and all facets of care. The plan mirrors South Australia's Generational Health Review, which mooted a joint Federal/State Commission.
The public health system has become increasingly dysfunctional, health care services are rapidly deteriorating, whilst the Canberra state divide has become a major barrier to reform. What is needed are fresh ways to end state-federal fights over funding that is based on divided responsibilities
We also need to address the divisions between hospitals and community care. Current funding is based on hospital bed use when the trend was towards reducing hospital stays. And there is a need to reduce dependency on hospitals and maximise preventive care by doctors and community-based services.
The background to this move for reform is this. It gave rise to this, which was based on the papers of the 1993 Health Care Summit
It was in this context that I read Julia Gillard's speech to the National Press Club. After saying that Australians want a world-class health system with a universal Medicare at its centre Gillard says that:
"Australians know our health system needs reform, real reform. The Howard Government knows that real reform is required - but instead they go for band-aid solutions, because deep down they do not want and are philosophically opposed to Medicare. They want to dismantle it, and they will - if they are re-elected. Saving Medicare and implementing real health reform can only be done - and will only be done - by a Latham Labor Government."
Most of the speech is political in tone and intent as it is concerned to paint a partisan picture of how the Howard Government promises a lot but delivers nothing eg., calling Medicare Plus Medicare Minus.
So what does Gillard propose by way of real health reform other than saving Medicare?
She mentions the ALP plan to get doctors bulk billing again, their Australian Dental Care plan to get half a million Australians off dental waiting lists and into dentists' chairs, and their plan to bring Medicare Teams of doctors and nurses to health hotspots around Australia.
That looks more like conserving Medicare to me than real health reform.
There is a commitment to the principles of primary health care, a recognition that burden of disease in modern Australia lies in chronic conditions such as mental health, and the end of cost shifting through a pooling state and commonwealth money.
Good ideas. Can the ALP deliver? Will the hard hearted straightners in the ALP stand aside for the reformers?
Posted by Gary Sauer-Thompson at 2:13 PM | Comments (2) | TrackBack
March 9, 2004
a small step
This story by Mark Metherell in the Sydney Morning Herald breaks new ground in the saga of Medicare.
Metherell's story refers to the broadening of Medicare to include dentists among the allied health professionals who will be incorporated in Medicare. Metherell says that Medicare benefits would be offered for needy patients with serious oral disease. He says that the dental scheme could operate as part of a extended health care program.
That is a significant move. Yet it is a small step in recovering the national dental scheme that was dumped by the Howard Government in 1996. As Mark Schifter writes:
" An oral health national strategy would entail that money is not simply flung at repairing and replacing teeth, but addresses the major cause of oral health dysfunction - tooth loss. In children and young adults tooth loss is primarily due to dental decay, but in adults, it is due to gum and periodontal disease, and the lack of a workforce to provide oral health care."
Incorporating dental health into Medicare is a good equity step since access to oral health services distinquishes the haves from the have-nots. A first step is an immediate injection of money.This step is needed for the disastrously long waiting lists (some more than five years) for basic dental services, for the relief of pain and the repair and replacement of teeth.
On Occam's Razor Patrick Shanhan said that the States are responsible for dental services and they had received an extra $2.5-billion from the Commonwealth. But that was spent propping up the health system, public dental services were cut back. Patrick says:
"The real issue here is not public dental services, but flawed national health policy, and its legacy....Dentally, more older people are keeping their teeth now, but they go to the dentist less often. The resulting dental neglect increases the medical risk and the likelihood of having to use more health resources. Despite this, oral health is excluded from healthy ageing programs.When you include oral health in health care you are not practicing dentistry, but preventive medicine."
The Commonwealth Dental Scheme introduced by Labor, was commendable, but it only addressed those on public dental waiting lists. It had no preventive component, and the high risk groups were excluded.
Posted by Gary Sauer-Thompson at 4:56 PM | Comments (2) | TrackBack
February 25, 2004
cracks in the health system?
Health continues to bubble along as an central issue in public policy circles. It's an issue that continues to favour the ALP. Bulk billing rates are declining; doctor's costs are rising; and attendances at doctor's practices are down. So what is going on here? What is happening if people are not going to see the doctor when they are sick?
Some---concessional card holders----are accessing the emergency departments of public hospitals. The others? The inference is that many of the working poor are not accessing the public health system. But it is not as simple as bulk-billing rates are disappearing and more people are turning up at hospital casualty departments, placing greater financial strain on a system funded federally but administered at state level. It means that people remain sick until they are faced with an emergency.
Here is the speech of Julia Gilliard, the ALP's Shadow Minister for Health, to the Australian Financial Review's 6th Annual Health Congress.
The AMA says that the key to evaluating our health system for patients, is being able to see a doctor when we need one.
Well, they've got that right. Speaking at a speech to the Financial Review's 6th Annual Health Congress Bill Glasson, the President of the AMA, goes on to say:
"ItÆs not as easy to get hold of a doctor when you need one these days, especially in country or outer-suburban areas. The concept of universal access to health care has eroded. Many Australians are paying more for their health care because Medicare has been neglected. But it doesnÆt have to be that way. If we can find money for border protection and offshore detention centres, we can properly fund our health system."
That is a perspective that is widely shared by public opinion. Whilst the Howard Government talks about spending the budget surplus on tax cuts, the majority of Australians (around 72%) want the budget surrplus to be spent on health and education.
Glasson then socks in the hits:
"Medicine has traditionally been the top of the heap of career choice for our best and brightest students.That reputation is slipping away.
Why?Too many bloody hurdles. Too much intervention.
The doctor-patient relationship does not want or need a Treasury official as note-taker. The doctor-patient relationship does not need the ACCC to brand rosters and job-sharing as anti-competitive. Student doctors should not be press-ganged into serving in country areas. A doctor should practice where he or she wants to practice, but incentives are needed to attract them to work in more remote areas.Red tape is strangling general practice. The Medicare patient rebate is dudding the patient.
These are causing massive damage to the system."
This is the restrained response by Tony Abbott, the federal health Minister. The Howard Government is doing a good job of managing the massive health system in a responsible and innovative way, despite the expense and cost blowout.
However, Abbott is reported in The Australian as being more provocative. He is reported as saying (p.5) that instead of the states laying blame on Canberra for the things that go wrong, the states should hand responsility for health to the commonwealth in the spirit of co-operative federalism.
Posted by Gary Sauer-Thompson at 5:04 PM | Comments (8) | TrackBack
February 17, 2004
Health: the politics of fear
Listening to Radio National this morning I was suprised at how the political topics of conversation had changed. It's health, education and work/family with terrorism, defence and the national security state now hovering in the background.
Health policy is going to become a key election issue. It's a strategy by the Howard Government to cut the ground from under the ALP; to claw back the traditional advantage of the ALP on this issue.
Now sitting behind the froth and bubble of the election sound bites is the Federal Treasury's Intergenerational Report (2002), which estimates a doubling of federal money on health over the next 40 years due to the aging of the population and new technology. That effect of the process of aging on health means big pressures continuing to build up on public funding of health care. That means health costs will have to be maintained once the election is out of the way.
My interpretation of the Intergenerational Report is that it is is going to be used to drive policy after the election. It begins to lay the groundwork for the 4th term policy agenda, and that goundwork has been carefully prepared in the name of fiscal sustainability. This is the prognosis: slower economic growth over the next four decades, lower productivity are forecasted; spending is projected to exceed revenue after 2014 largely because of health and ageing; and that means higher taxes or reductions in government spending.
It's an overload thesis. Sound management is required. So we have to cut health spending on Medicare and PBS (in small steps) over the next decade.
This raises the corollary issue of the public funding of private hospitals through private health insurance (rebate and lifetime cover). Why this mechanism? Should we not question this way of funding in the name of economic efficiency?
It seems to be an axiom of politics that a public subsidy ($2-$3.3 billion) of private health insurance must be maintained in order to sustain the private health system. Without the 30 per cent rebate and lifetime health cover private health insurance would fall to very low levels. The private health insurance industry would collapse, and federal government budgets would come under enormous pressure. So private health insurance shifts the burden of health service delivery from the public to the private sector.
It's the fear argument. Ignore the fear rhetoric and one can see that there are other ways to fund private hospitals. It is no longer the case that reducing subsidies for private health insurance is doing away with the private health system. That is the line of the private health insurance industry.
The private health insurance industry is a high cost financial intermediary protecting its corporate welfare.
Why not fund the private health hospitals directly--say through a bed subsidy? Why not cut out the private health insurance industry? Take its snout out of the public trough, and force it to stand on its own feet and embrace the discipline of the market.
The problem is not Medicare. It is the private health insurance industry. Subsidizing the insurance industry is a high cost way to fund the services provided by private hospitals. It sucks up a lot of the public subsidy to run itself.
The article on health policy, 'A healthy use of public funds', by Ian Harper and Chris Murphy in today's Australian Financial Review (subscription required, 17 02 04, p. 55) defends the public rebate of private health insurance. It amounts to a defense of corporate welfare for the public health insurance industry, under the guise of limiting the looming blowout in government health costs.
Defending the corporate snout in the trough is a rather strange line of argument for hard nosed neo-liberals who love the free market. Isn't the market meant to be about the survival of the fittest?
Maybe these hard nosed neo-liberals have gone all weak in the knees. Or maybe these economists don't know that much about health.
Posted by Gary Sauer-Thompson at 10:02 AM | Comments (9) | TrackBack
February 12, 2004
Senate: Medicare Plus
There is a political judgement buried in the daily media flows that a deal will be done over the Howard Government's Medicare Plus. What has been introduced into the Senate today is the safety net legislation that is part of the revised $2.4 billion Medicare Plus package.
The political background to this legislation is the Howard Government's slow strangling of Medicare and public hospitals over the last 7 years and MedicareÆs continued popularity with Australian citizens. The Howard Government has continued to cry poor when funding Medicare, public hospitals and subsidised medications. It argues that the costs are becoming too great for any government to bear, hence the need for co-payment (out-of-pocket charges at point of service). Yet the Howard government happily pours ever increasing billions into the private health system. Medicare is worth defending despite the problems of uncapped fee-for-service medicine and inadequate rural medical services.
Abbott's MedicarePlus legislation is quite narrow. Most of the Package was implemented through regulation. It involves thresholds for all Medicare health expenses (safety net). The thresholds are $500 and $1000. Once reached an 80% rebate comes into play. The $500 threshold only applies to concession card holders and lower middle-income earners, whilst the $1000 threshold applies to everyone else.
Will the working poor be able to afford the $1000 of medical expenses? Is the effect of the rebate on specialist fees inflationary?
I was able to catch a bit of the Senate debate on Medicare Plus this morning. I'm trying to get a sense of how it all works. How are the deals done? What actually takes place in cutting a deal? How do the deals relate to the Senate debate?
There seems to be a ritualistic political debate between the Coalition and the ALP Senator's going on over safety net versus universal health system. I saw a bit of Senator Linda Kirk is more reasonable in presenting the ALP case. Of all the speakers Ursula Stevens was the most informed about the issues involved.
I saw nothing in the media about the negotiations. All I that I can see is the public debate in the Senate, which finished around lunchtime. The negotiations take place behind closed doors away from the public eye of the media. All we have is the odd news reports. One states that Tony Abbott is saying that he has ruled out making concessions on the Medicare safety net that were not in line with Government policy. Another states that the Independents are saying that they were keen to see Medicare returned to a universal health care system.
At the end the day nothing much had happened. Early reports said that negotiations were continuing and that progress was being made. That bland statement says nothing about whether the Independents have managed to pull Medicare Plus back to a universal health care system, let alone introduce some innovation into Medicare to break the doctor/drug style of medicine.
Update
Media reports on Friday morning represent Abbott as saying that he was frustrated but confident. He was going to the hard work to get his package through. Abbott is looking at the Independent Senators proposal to extend allied health (podiatry, physiotherapy and dietics) to more people under Medicare. And so he should. It is innovative.
The ACTU is reported as saying the legislation should be blocked in a last ditched stand to save bulk billing. They do make some good points about the discrimination towards singles and the working poor in the Medicare Plus package.
However, the "Custer's last stand" means that everyone should side with the ALP. The ACTU assumption is that only the ALP has the right policies on health. Anything that is not in accord with the health policies of the ALP represents a sell out.
Why not good criticism of the public subsidy for the private health insurance industry. A large percent of money passing through private health insurance failsv to make it to private hospitals - it goes onancillary services, excess "gap" payments to medical practitioners, and to bureaucrats in the private health insurance industry. A criticism of subsidizing private insurance that accepts supporting private hospitals.
Why not a few ideas on how to bust open the power of the doctor cartel as well? Many Australians go to allied health professions to seek help for their aching wounded bodies. Why cannot we open the door to a multidisciplinary course of treatment under Medicare? Why not a broader conception of primary health care, which is the most important sector of any health system.
Posted by Gary Sauer-Thompson at 10:11 AM | Comments (7) | TrackBack
December 19, 2003
SA health politics: The Advertiser
In an earlier post on the ongoing health crisis in South Australia I briefly described the politics of the Murdoch-owned Advertiser as being gullable for the swallowing the Minster's line. I also said that it's journalists were content to recycle media releases instead of doing investigations.
There is a long tradition of this in Australia. Did not Bjelke Peterson, the ex-Premier in Queensland, call it feeding the chooks? From memory, Paul Keating, the ex Federal Treasurer, called it putting the journalists on the drip feed.
I've changed my mind about my representation of the politics of The Advertiser. It is more than bootlicking by media whores. It's management has decided to use the recent symptons of the systemic crisis of the public health system to bash the bureaucrats. That is politics of the Murdoch media in Adelaide.
The Advertiser holds that the bureaucrats in the Human Services Department cannot balance their budget. The Department is run bytoo many over paid fat cats. The inference? The budget is in the red because of overpayment of highflying executives. The conclusion? We have six years of budgetary mismanagement. Those highflying executive fat cats need to to be taken out.
That --"bash the bureaucrats"---is the frame they put around the Rann Government's crisis management flowing from years of budget cuts. And the media hacks running the Rann media machine would be pulling out the champagne corks.
The reality is otherwise.
The decades of budgetary cuts have seen the hospitals being run down. Their normal condition is no capital works, outdated equipment, decaying buildings. The public hospitals are out of date and run down.
Of course, the Rann Government's spin is that it is doing all can. It was the previous Liberal Government who let things slip. But the state budget is tight.
The line is not even questioned by the media whores at The Advertiser.
Posted by Gary Sauer-Thompson at 2:16 PM | Comments (2) | TrackBack
December 18, 2003
SA politics: health crisis
After all the cuts, restructuring and reorganization made to the SA Department of Human Services over the last decade, a financial black hole has been discovered by the Rann Government along with the financial irregularities. The Department has been overspending and is need of a bailout, says a senior Government source drip feeding a gullable Advertiser, It's journalists recycle media releases instead of doing investigations.
Chris Sheil over at Backpages puts it well:
"I've seen it many times. Decades of re-organisation and rationalisation will eventually catch some sucker; the one who's sitting in the chair when the thing falls over. Under the longstanding neo-liberal policy influence, just about the only definitive way that governments can discover their services are stuffed, is by default. It's not uncommon to find a minister's portfolio predecessors joining in the scalp hunt, despite being equally, and sometimes even more, culpable."
Well things have fallen over at the Department Human Services with "emergency" funding needing to put in to keep things ticking over.
Emergency means that there is a systematic crisis here, due to a couple of decades or more of cutbacks to health by both Liberal and Labor Governments.
The solution? For the Rann Government it is to restructure the Human Services Department yet again. Thus the Treasurer, Kevin Foley, says:
"This Government is smashing a large, unwieldy bureaucracy and making two leaner workplaces that will be more service-focused.... We decided to split it in half so we can have an agency looking after health specifically and an agency looking after family and community services and protection of our children and the ageing."
That imagery of "smash" and "lean" about the health bureaucracy is neo-liberal imagery. It means more cut backs, more job cuts, less services, doing more with less. The "more service focused" image is the human face that says we are still a Labor Government and we care. Both together means that no attempt is to be made to deal with the systemic crisis in health.
How do you deal with the systemic crisis? Chris Sheil has one solution. He says:
"The first thing you do is reverse the present Australian government responsibilities. Hospitals should be directly funded by the national government, just like universities. The closer people come to dying, the more health-monies are consumed. Hospitals are the deep end of the system; the big health factories; the catastrophic centres; the places where the real big bucks go, just before people go off to meet their maker. The Australian federation has a pronounced vertical fiscal imbalance, which should dictate the distribution of government responsibilities, and this rule says that there should be direct national hospital funding."
Sounds more like aged care to me. Why not more aged care facilities for the dying than using hospitals for this purpose? The Commonwealth already pays for aged care and primary health care. Why not give the states a bundle of money and allow them to spend it as they see fit within specific criteria to ensure they are accountable?
The states have the money as the GST is now flowing to their coffers. SA is getting more than it expected from the GST ($230 million) and it is expected to be GST positive before 2006-7. The Rann Government has the money to spend on health, but it refuses to do so. It stands for "prudent management" as defined by the criteria of the money market.
Posted by Gary Sauer-Thompson at 1:30 PM | Comments (2) | TrackBack
December 9, 2003
there's evil in that big place on the hill
By all accounts this article by Greg Barnes is pretty accurate in terms of its descriptions of the working environment of Federal Parliament. Barnes says:
"Parliament House is a brutal and unrelenting work environment. It warps people's judgement. Issues and information that bear little or no consequence to reality suddenly become important. The media, staff members and politicians feed off this poisonous atmosphere in a building that contains some fine art and architecture but no soul and no warmth.
To expect people to work 16-hour days day in and day out in such a place is unfair and downright cruel. And to expect them to do it in a city such as Canberra, where there are few support networks, little sense of community and no capacity to escape, means that the mental health of those who work in the House is put under such intense pressure that drugs, alcohol, sex and workaholism often come to be seen as the only means for survival."
This political hothouse is a place for those young singles who love the nomadic, homeless existence and find the throb of political power orgasmic. It is hell on relationships and families, as you can well imagine. You survive by leaving.
Barnes describes the way the atmosphere of Parliament is determined by the nature of politics as an existential conflict between friend and foe:
"The game of politics as it is played in Australia is needlessly cruel and primitive. People's foibles, misjudgements and handicaps are not the subject of empathy or sympathy but of derision....Perhaps most importantly, it is virtually impossible for MPs and staff members to find a shoulder to cry on, to talk frankly to someone else simply as one vulnerable human being to another."
All of this is well known. The stories I've heard suggest that Old Parliament House had a more collegial atmosphere. By contrast the new building has an:
"....an environment that takes no prisoners, that refuses to change its work hours to make them less stressful and, above all, that has no regard for the mental health of individuals who are often fragile but ambitious and narcissistic by disposition, in any event."
Senator Brian Harradine had it right. It is a place with evil in it. There is an intensity of experience there that is brutally destructive. You end up in paranoic snarling mode that cannot be controlled.
Tim Blair and his cohort of callous readers can only mock those staffers who suffer from the brutal work conditions. Mocking the misfortune of others is called humour by these mediocre snivellers, who are so envious of their masters for their rank, nobility and breeding.
Posted by Gary Sauer-Thompson at 10:37 AM | Comments (3) | TrackBack
November 27, 2003
the politics of medicare
In this piece in the Melbourne Age Kenneth Davidson says "I can't see why MedicarePlus is a political winner for the Howard Government. It does nothing to address the fundamental issues that concern voters about the Government's duplicity in its management of the health portfolio."
At one level the answer is simple. As Laurie Oaks writing in The Bulletin says MedicarePlus is a political package designed to provide the Coalition with political cover. It is designed to neutralize an issue that the ALP was starting to use to its own advantage. And Howard has probably succeeded in defusing health as a political problem for the Coalition.
MedicarePlus is not designed to address the fundamental issues that currently plague public health. It exposes Crean even more, puts more pressure on the ALP, feeds the conflicts within the ALP, and helps to keep the ALP demoralized at the prospect of another three years in opposition. Buying Senate support keeps the ALP on the ropes.
Davidson is right in his judgement that:
"The Howard Government (and the Fraser government before it) has been undeviating in its central health policy objective: to undermine the universal character of Medicare (and Medibank before it) and turn it into a safety net for the poor..."
The popularity of Medicare amongst Australian citizens means that it is difficult for right-wing governments to reverse the social democratic public health system, turn it into a two tier health system, and transform Medicare as a form of welfare. The political strategy is to characterise Medicare and bulk-billing as a system for the poor. This would then justify Government underfunding of the public health system, and legitimate tax cuts for those who refuse to acknowledge that health is a public good that should be paid through taxation.
We can read the politics of MedicarePlus in terms of electoral strategy for the next federal election. Howard is buying Senate support for bills that would count as a double dissolution trigger. He is avoiding a double dissolution election because it would weaken the Coalition's post election numbers and return more Australian Greens to the Senate.
Posted by Gary Sauer-Thompson at 1:43 PM | Comments (1) | TrackBack
November 19, 2003
Medicare
Judging from news reports it would seem that the Howard Government is willing to spend big enough on public health (from $917 million to $2.4 billion) to neuter health as an election issue favouring the ALP. By all accounts the revamped package (dubbed MedicarePlus) has enough goodies (paying GPs an extra $5 to bulk-bill children; more doctors and nurses) and concessions (an expanded safety net for low and middle income families) to ensure that it will pass the Senate within weeks.
Health was a key negative issue for the Howard government with voters in the lead-up to the federal election. It has been addressed with buckets of money replacing the old modus operandi of bashing the Senate for its wilful obstruction has been quietly dropped.
Much of the Package will go through the Senate under ministerial regulation rather than legislation. Louise Dodson explains the strategy:
'By using regulation to get key parts of the package through the Senate, the Government has made it difficult for opposition parties to influence the new package because they will be presented with a "yes" or "no" choice on topics such as incentives for doctors to bulk-bill children of low-income families. The strategy does not give them the chance to propose amendments. Saying "no" to many of the proposed changes would be political suicide.'
Despite the modest investment MedicarePlus is a political winner as it leaves the Opposition Labor Party with little room to move.
And so the federal election has begun. Medicare is safe with the Howard Government is the political message.
Given that the incentives for doctors to bulk-bill are restricted to welfare recipients and children, the MedicarePlus package continues the trend towards a two-tiered health system: private health for the rich and public health for the poor. We already have a two tiered health system where wealth does buy better access and the user-pays principle that is replacing bulkbilling.
The long-term strategy of the Howard government is to push as much of health care spending off the federal budget----shifting to private health insurance. That is the right and proper policy intones the editorial in the today's Australian Financial Review (subscription required, 19 11 03, p. 70). The Howard Government is making the shift through a policy of eroding Medicare through shifting costs to patients. It does this in MedicarePlus by refusing to put public money into bulk billing for all citizens and by targeting concessions to specific groups. For the spin on this see Chris Sheils' Back Pages.
It is also doing little to reform the market for health-care services.
Posted by Gary Sauer-Thompson at 10:54 AM | Comments (7) | TrackBack
October 10, 2003
just a few porkies
In The Bulletin this week Maxine McKew has lunch with John Dwyer, who fronts the Australian Health Reform Alliance. Dwyer talks a lot of sense about the current health crisis.
It is a crisis. It cost Kay Patterson her job. She was cut loose. Health becomes a major debacle on several fronts for the Howard Government. Aged-care, remember, has already chewed up Judi Moylan and Bronwyn Bishop. That rising star, Julie Bishop, is the fifth minister responsible for aged-care since 1996.
The Australian Health Reform Alliance was formed when it seemed that the reform agenda had been lost. The Commonwealth and States and Territories had lost the plot on health reform as they started to squabble amongst themselves. Things were becoming dysfunctional in the health system.
Dwyer highlights a key reason for the overloading at public hopitals. He says that:
"... on any day, overloaded public hospitals (funded by the states) are dealing with emergency or geriatric patients who could otherwise be cared for in (federal-funded) GP health centres or nursing homes. An example: nearly every day during the past Łwinter, the Prince of Wales was forced to turn away ambulances, including those Łcarrying patients with life-Łthreatening conditions, because of overflowing Łemergency departments."
He then mentions three ways in which the Howard Government has been consistently telling porkies when it comes to the public health:
"The first porky is that the government's changes to Medicare are designed to make the system fairer. That is definitely untrue."
It is untrue because the reform package, is designed to prop up bulk billing for the poor and elderly but effectively makes it easier for doctors to charge the rest of us more. That does not lead to equity of outcome. It is not a question of money. A $5 pay rise for an average GP consultation costs the taxpayer $500m. Recently there was $2bn spent on the 'hamburger' tax cut. This is about values not money.
The second porkie Dwyer mentions is
"....the bald-faced statement from the prime minister that the private insurance rebate is taking the pressure off public hospitals. If there was any blip of help initially, it's long since gone. What the PM is doing is confusing increased activity in the private hospitals and making an incorrect linkage. As we all know, lots of Australians, no matter how wealthy, are in public hospitals because that's where the sophisticated services are. All the health economists can demonstrate this to any impartial person's satisfaction. Equally, there are plenty of ways that we could better use the money that's now propping up private insurance to also help the public system."
Again, it's about values not money. The aim of using $2.4bn a year on federal finances is to faciliate private health industry and to run down public health system.
The third porkie? It is
is the PM's constant refrain that if the public hospitals are a mess, then it's a state responsibility. The message we've tried to get through for months is that what happens to primary care affects hospitals and vice versa. In health, integŁration is everything. If GPs in a certain area aren't earning enough money to operate an after-hours service then we'll immediately see increased numbers in emergency wards in hospitals. The same if there aren't enough nursing beds. This is not to let the states off the hook either. They need to be far more transparent about everything. The fact is it's totally irresponsible for either the federal or state governments to talk about the issues as if we're dealing with islands of health care."
What we can say is that the Howard Government is not commited to fixing a dysfunctional public health system. As we see with medical indemnity insurance it will endeavour to politically manage the situation to ensure its re-election by preventing an electoral backlash. It is more interested in buying time and de-politicizing the issue Ithan ensuring a vibrant and universal public health system. It's vision is one of a health system run by big corporations making a profit, whilst the public health system is transformed into charity hospitals run by nuns and volunteers.
The Howard Government would really like to get out of public health. If it could, it would repudiate the egalitarian heritage of social democracy. Its policies of more and more deregulation and less and less social spending indicate a continual retreat from egalitarianism, despite the community's support for most types of social spending through the provision of public services. This is particularly the case in health.
The papers from the Alliance's recent health summit can be found here.
Posted by Gary Sauer-Thompson at 9:22 AM | Comments (3) | TrackBack
October 8, 2003
a new political wind blows
 One achilles heel of the Howard Government is its attempts to undermine the public health system through a drip feed. Why spend good money on something that is bad?
One achilles heel of the Howard Government is its attempts to undermine the public health system through a drip feed. Why spend good money on something that is bad?
Clearly, self-reliance was the way to go. The democratic mass needed to be toughened up. They had been sucking on the welfare tit for far too long and had gotten used to it. What was needed was to reduce bulkbilling to only the deserving poor, and then use the money to subsidize, and prop up, the private health funds.
The politics was to keep just enough blood flowing to the public heel via the old drip feed to prevent gangrene and keep the system on its feet. That would keep the masses quiet long enough to retain power. Hopefully, the private health system would grow in a globalized world with massive corporate welfare. Gee, maybe even the American corporations would take things over. Why, a free trade agreement would help to keep the health reforms ticking along.
The proposed reforms to public health had no chance of getting through the Senate in their current form. The Senators understood that more money was needed to be pumped into Medicare, and that a higher Medicare rebate was needed for doctors to encourage them to bulk bill. Equity in health care still meant something in the Senate: it meant a just health care system, one in which all people have the right to be treated equally by government policy and financial assistance schemes.
In the process of holding the pro-market, anti-governmental line the Howard Government has taken a PR hit-----big time. It was seen to actively creating a two-tier health insurance system, with bulk-billing retained only as a safety net for the poorest Australians. Despite the rhetoric of creating æa fairer MedicareÆ, whilst restricting access to health care (with financial barriers for a significant proportion of the Australian population) the Howard Government was seen to be politically opposed to a public system of universal cover for sickness. The future was a going back to the philosophical principles of the pre-Whitlam health care system.
Are we are now seeing a change in tack? Just like we did in early 1991 first half of 2001 when a spooked Government went on an expensive exercise in vote buying. In late 1993 in steps Tony Abbott, the new man from the Government with a conciliatory tone, a big smile and buckets of cash to save the day. The new Liberal hero and future Liberal PM.
I reckon we are seeing a change of political tack. A new political wind is blowing. Health is a crucial issue in the forthcoming federal election.
Michelle Grattan thinks so too. Don't you love the image. Tony Abbott as the pest control man knocking off the democratic voices. That's political conservatism for you: govern through the free market and keep squeezing democracy to ensure that citizens are passive outside elections.
Posted by Gary Sauer-Thompson at 4:53 PM | Comments (0) | TrackBack